In this study, we retrospectively reviewed the penile color Doppler ultrasound (PCDU) scans of the patients who had admitted to our clinic with erectile dysfunction and aimed to evaluate the contribution of penile Doppler scan results to the clinical decisions.
Material–methodThe data of patients admitted to our outpatient clinic with complaints of erectile dysfunction (IIEF-5 score<22 or IIEF-EF score<26) between January 2005 and January 2018 were retrospectively evaluated. Patients whose testosterone level is lower than 280ng/ml or who had undergone radical prostatectomy were excluded from the analysis.
ResultsThree thousand ninety patients were included in the study. The mean age of our patients was 55.05±13.05 years. In total, 2139 (69%) patients had normal PCDU findings, 351 (11%) patients had arterial insufficiency, 531 (17%) patients had venous insufficiency, and 69 (2%) patients had arterial insufficiency with concurrent venous leakage. When the patients were divided into 2 groups ≤40 years (Group 1) old and >40 years (Group 2) old; normal PCDU findings were found in 432 patients (84%) of the Group 1 patients and normal PCDU findings in 1707 (66%) patients of the Group 2 patients (p<0.0001). There were arterial insufficiency findings in 24 (4.7%) and 327 (12.7%) patients of the Group 1 and 2, respectively (p=0.002).
ConclusionThe etiology is psychogenic in the majority of patients who present with ED complaints to the urology clinic. With age, the prevalence of psychogenic ED is decreasing but still more than organic.
En este estudio, revisamos retrospectivamente las ecografías Doppler a color del pene (PCDU) de los pacientes que ingresaron en nuestra clínica con disfunción erectile, el objetivo era evaluar la contribución de los resultados de la ecografía Doppler peneana a las decisiones clínicas.
Material y métodoLos datos de los pacientes ingresados en nuestra clínica ambulatoria con quejas de disfunción eréctil (puntuación IIEF-5<22 o puntuación IIEF-EF<26) entre enero de 2005 y enero de 2018 se evaluaron retrospectivamente. Los pacientes cuyo nivel de testosterona fuera inferior a 280ng/ml o a los cuales se les hubiera realizado una prostatectomía radical se excluyeron del análisis.
ResultadosEn el estudio se incluyó a 3.090 pacientes. La media de edad de nuestros pacientes fue de 55,05±13,05 años. En total, en 2.139 pacientes (69%) hubo hallazgos normales en la PCDU; en 351 (11%) se observó insuficiencia arterial; en 531 (17%) insuficiencia venosa y en 69 (2%) insuficiencia arterial con reflujo venoso simultáneo. Cuando los pacientes se dividieron en 2 grupos, ≤40 años (grupo 1) y >40 años (grupo 2), se encontraron hallazgos normales de la PCDU en 432 pacientes (84%) de los pacientes del grupo 1 y hallazgos normales de PCDU en 1.707 pacientes (66%) del grupo 2 (p<0,0001). Hubo hallazgos de insuficiencia arterial en 24 (4,7%) y 327 (12,7%) pacientes de los grupos 1 y 2, respectivamente (p=0,002).
ConclusiónLa etiología es psicógena en la mayoría de los pacientes que presentan quejas de en la clínica de urología. Con la edad, la prevalencia de la DE psicógena va disminuyendo, pero todavía es más psicógena que orgánica.
Erectile dysfunction (ED) is a major issue in the men's health with a significant effect to the quality of life. It was described as inability of obtaining and maintaining a satisfactory erection for sexual intercourse.1,2 Due to the results of The Massachusetts Male Aging Study, 52% of males between 40 and 70 years of age have some degree of ED.3 Two main etiological groups of ED, organic and psychogenic, are commonly accepted in the contemporary literature.3 Organic etiology can be further classified into vascular, neurological, endocrinological, and anatomical factors.2,4
ED is more common as a symptom in the aging male.5 Thus, it is coincident with other comorbidities which are also common in the aging population such as hypertension (HT), atherosclerosis, diabetes mellitus (DM), and hyperlipidemia (HL). Considering the well-known role of endothelial dysfunction in the pathogenesis of ED, it can be assessed as the early sign of an upcoming cardiovascular event.6
The management of ED largely depends on using phosphodiesterase type-5 (PDE-5) inhibitors, either daily or on-demand. Intracavernosal injections provide the second-step options while penile prosthesis implantations are ensuring a mechanical solution to the issue in the last-step. The evaluation of the patient is made by anamnesis, blood lipid and glucose profile, testosterone assays, nocturnal penile tumescence test, and penile color Doppler ultrasound (PCDU) scan. For the vascular etiologies PCDU holds its indispensable place and vascular factors can be excluded in case of a normal PCDU scan result.3
However diagnostic accuracy of PCDU finding in term of ED's etiologic factor is still controversial. In elderly patients, vascular pathology is generally blamed as etiologic factor of ED, whereas psychologic factor is the culprit in young male. In this study, we aimed to assess the distribution of vascular pathologies and psychogenic ED in the entire cohort of patients who had evaluated for ED in our clinic.
Materials and methodsThe patients who had admitted to our clinic with the complaint of ED and IIEF-5 score lower than 22 or IIEF-EF score lower than 26 are retrospectively reviewed. The present study protocol was reviewed and approved by the institutional review board of Ankara YıldırımBeyazit University, School of Medicine, Ankara Ataturk Training and Research Hospital (Reg. No. 179). Patients whose serum testosterone levels less than 280ng/ml, has a neurological or psychiatric disease history, has an anatomic deformity and who have undergone a pelvic are excluded from the study. Total of remaining 3090 patients’ data were evaluated. Results of the PCUD scans, patients’ medical histories including the timeline of ED and comorbidities were interpreted from the patient charts and local databases. Moreover, the past medical histories for all patients with were reviewed from the patient charts. Considering the normal testosterone levels and lack of any past medical history, patients without vascular disease in PCUD were accepted as psychogenic ED. The patients were divided into two groups using the 40 years of age as the cut-off point. Group 1 (n=513) comprised the patients who are younger than 40 years of age, while the elder patients were ingathered in Group 2 (n=2577).
Technique of PCUD scanGray-scale US and Doppler US examinations were performed with a Logiq S7 Expert machine (GE Healthcare, Milwaukee, WI) equipped with a 9L-D linear-array probe. In the examination room, with the patient lying in supine position and the penis held in the anatomical position, 2ml (60mg) of papaverine was injected with an insulin injection needle into the lateral aspect of the proximal third of the right cavernous body via US guidance under sterile conditions. On gray-scale US, probable lesions such as tunical plaques were evaluated by dorsal and ventral approach in longitudinal and transverse planes. After the injection, a dynamic assessment of the spectral Doppler waveform in the cavernosal arteries was performed on the proper Doppler angle at 30–60 degrees. Spectral Doppler US findings including peak systolic velocity (PSV) and end-diastolic velocity (EDV) were recorded, and the diagnosis based on Doppler US was determined. Post-injection measurements including PSV, EDV and visual maximum tumescence and erection hardness were taken from 0 to 20min. This sonographic examination was terminated after spectral Doppler measurements taken at the twentieth minute. The patients were warned about probable priapism. If the PSV value was below 25cm/s during the examination, the diagnosis was considered arterial insufficiency. When the PSV was ranged from 25 to 30cm/s, the diagnosis was considered borderline for arterial insufficiency. PSV values above 30cm/s were considered normal for arteriogenic function. When a good diastolic reversal or below 5cm/s EDV values were achieved during the examination, venous insufficiency was ruled out. When the EDV value was still above 5cm/s at the end of the examination, the diagnosis was considered venous insufficiency.7–9
Statistical analysisStatistical analyses were performed using SPSS version 15.0 (IBM Corporation, Armonk, NY). Descriptive statistics of continuous variables are given as mean±standard deviation (SD). To compare groups, Student's T and chi-square tests were used for normally distributed data. p<0.05 was considered statistically significant.
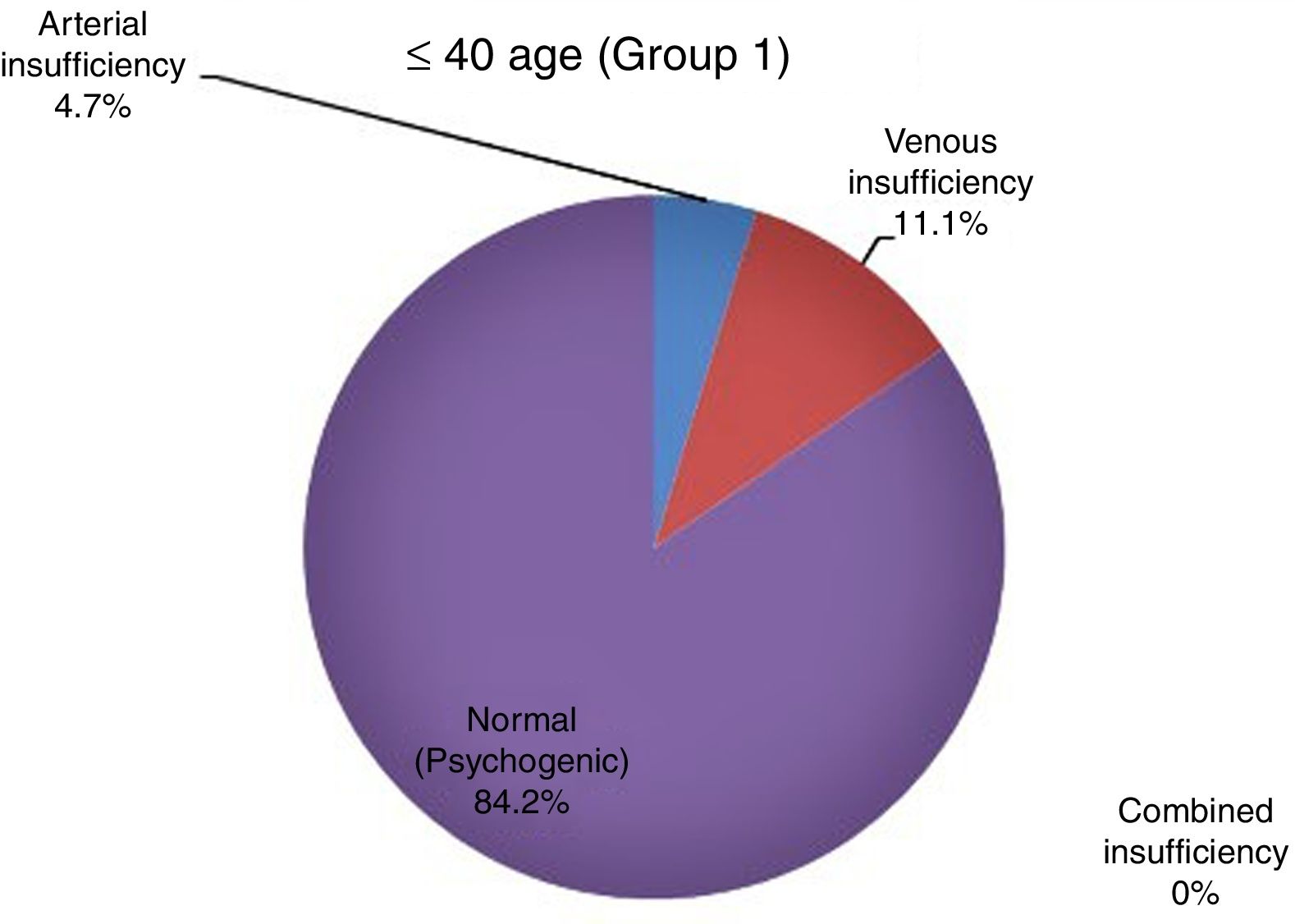
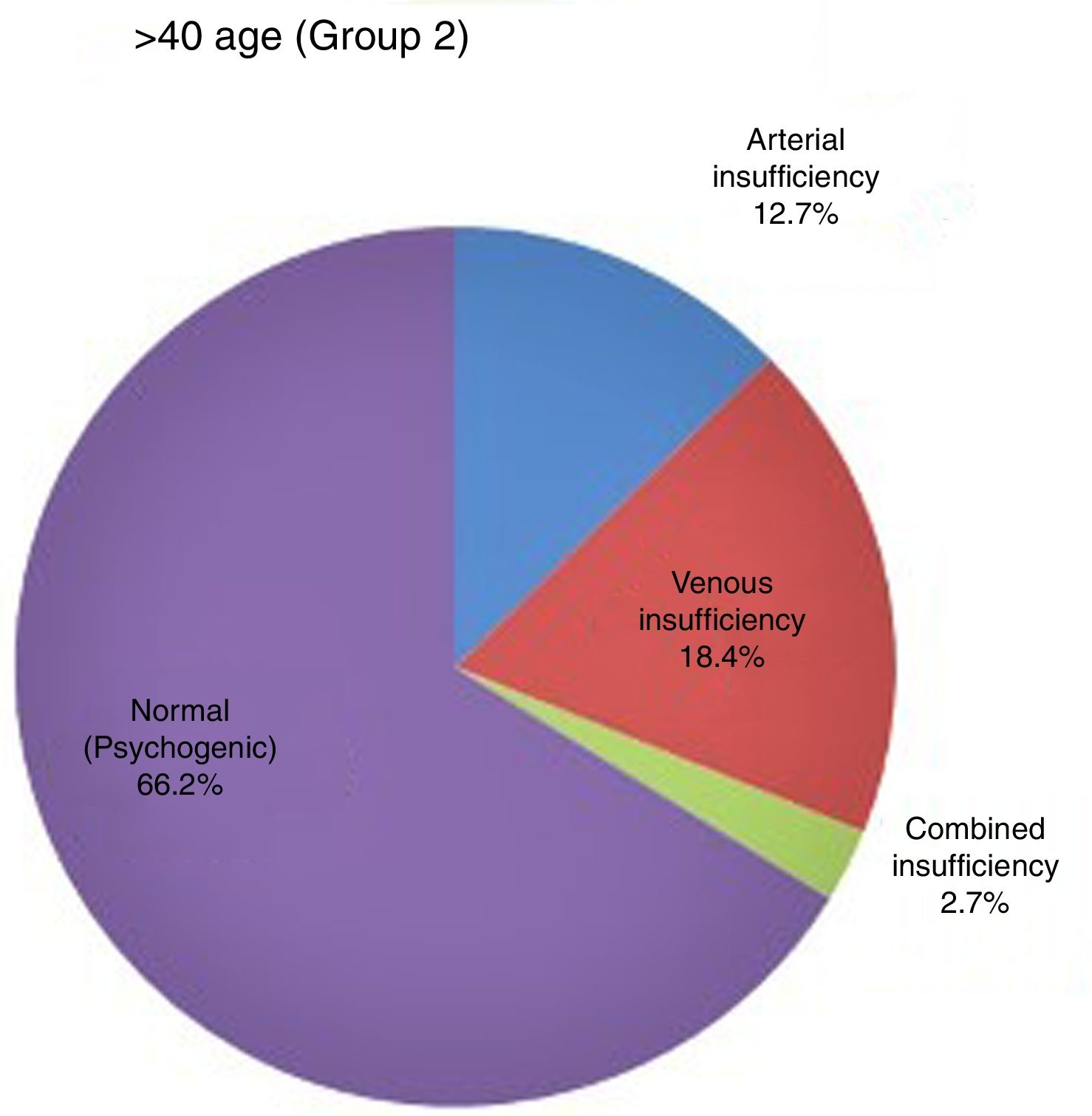
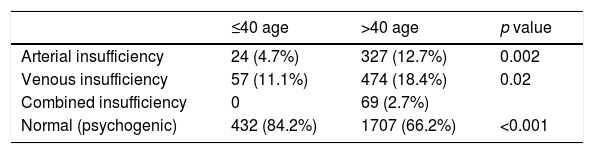
ResultsA total of 3090 patients (mean age, 55.05±13.05 years; range, 18–87 years) were included in the study. There were 513 patients in Group 1 and 2577 patients in Group 2. In the entire cohort, 69% (n=2139) of the patients had normal arterial and venous flow rates. Arterial insufficiency was observed in 11% (n=351), venous leakage was observed in 17% (n=531), while combined arterial and venous insufficiency was noted in 2% (n=69) of the patients. 432 (84.2%) patients in Group 1 and 1707 (66.2%) patients in Group 2 had normal PCDU findings and found statistically significant (p<0.0001) (Table 1 and Figs. 1 and 2).
Penile color Doppler ultrasonography findings and frequency in patients ≤40 and >40 years old.
| ≤40 age | >40 age | p value | |
|---|---|---|---|
| Arterial insufficiency | 24 (4.7%) | 327 (12.7%) | 0.002 |
| Venous insufficiency | 57 (11.1%) | 474 (18.4%) | 0.02 |
| Combined insufficiency | 0 | 69 (2.7%) | |
| Normal (psychogenic) | 432 (84.2%) | 1707 (66.2%) | <0.001 |
The incidence of arterial insufficiency 24 (4.7%) in Group 1 and 327 (12.7%) in Group 2 (p=0.002), venous insufficiency 57 (11.1%) in Group 1 and 474 (18.4%) in Group 2 (p=0.02) and concurrent arterial with venous insufficiency 0 patients in Group 1 and 69 (2.7%) in Group 2 showed statistically significance between the groups. Of the total patients, 2889 (93.5%) had no tunical plaque, while 201 (6.5%) had plaque. One hundred seventy-four (8.1%) patients with Peyronie's Disease had normal PCDU, 9 (2.6%) patients with arterial insufficiency, 12 (2.3%) patients with venous insufficiency and 6 (8.7%) patients with combined insufficiency were found.
Being classified due to the erection hardness score, after the intracavernosal papaverine injection 26.5% and 33.2% of patients could initiate and maintain grade 4 and grade 3 erection, respectively, while 10.8% and 29.3% of the patients could only elicit a grade 1 and grade 2 erection, respectively.
Consequent of the PCUD scan, 129 patients with ED underwent penile revascularization surgery, 33 patients underwent penile prosthesis implantation, and penile revascularization with plication was carried out in 60 patients. In the penile prosthesis group we did not observe any complications and all patients were able to penetration in the third month postoperatively. Among 129 patients who have undergone penile revascularization, clinical success which is defined by being able to have sexual intercourse is observed in 71 (55%) patients, 7 patients were lost to follow-up in this group. Twenty-four patients (40%) in the penile revascularization with concurrent penile plication group were able to have a vaginal penetration that was reported to be satisfactory, and 3 patients were lost to follow-up in this group.
DiscussionErectile dysfunction has a multifactorial etiology and a wide pathogenetic background that involves endocrinological, vascular, neurological systems as well as psychological status of the patients. Contemporary approach of International Society of Sexual Medicine (ISSM) defines two main groups of ED respect to the etiology, organic and psychogenic ED. Psychogenic ED is characterized by a sudden onset with usually spared nocturnal erections. On the other hand, patients with organic ED etiologies usually lost nocturnal erections and have a gradually progressive symptom. In young males, ED is usually multifactorial and has both organic and psychogenic underlying factors.10
Organic factors leading to ED can be sub-grouped as vasculogenic, neurogenic, endocrinological, and anatomic. Vasculogenic ED is most commonly a result of atherosclerosis in elders. Atherosclerosis leads to diminished blood flow and endothelial dysfunction that further compromises the dilation capability of the vessels and cavernous trabeculae. Hypoxia induced fibrosis triggers a vicious cycle that may result total loss of the erectile function.11–13
Psychogenic factors can also have multiple components that is challenging to the clinician.14 In our study, we excluded patients with a history of neurologic disease, low testosterone levels, anatomical problems, and a history of penile surgery. By the exclusion criteria, we aimed to narrow down our cohort to psychogenic and vasculogenic etiologies. We then obtained a psychogenic ED diagnosis by excluding the vascular dysfunction using PCUD scans after intracavernosal papaverine injection. Using the well-defined cut-offs, we accepted the patients who have normal EDV and PSV values as psychogenic ED. In both the younger and the elder patients, psychogenic ED constituted in most of the cohort.
The prevalence of ED showed positive correlation with the age in previous studies. In a cross-sectional study from the US, prevalence of ED is found to be four times higher in men at their 70s respective to the men at their 20s. A multi-national survey that included 27,839 men showed 37%, 11%, and 8% prevalence of ED in men who are 70, 30, and 20 years old, respectively.15,16 In another study patients had grouped using 40 years of age as the cut-off, and all patients were evaluated with psychological examination, nocturnal penile tumescence test, and PCUD. This study included 948 patients whose IIEF scores lower than 21, and as a result 85.2% of the patients who are under 40 years of age were reported to have psychogenic ED. On the other hand, the prevalence of psychogenic ED was reported as 40.7% in the patients who are older than 40 years of age.17 Khanzade et al. group their 97 patients using the same 40 years of age cut-off and reported a higher incidence of psychogenic ED in the younger patients.18 Our results are compatible with the previous literature at this point. We observed significantly higher prevalence of psychogenic ED in the younger patients (84% vs 66%, p<0.001). However, we want to underline that the prevalence of psychogenic ED in the elderly group was not negligible.
To the best of our knowledge, we report the largest patient cohort to the date that involves differentiation of psychogenic ED from the vasculogenic etiology using PCUD. The primer limitations of our study were the lack of comprehensive psychological examination of the patients, and the retrospective fashion of the study. The secondary limitations are not being able to record predisposing diseases for ED such as diabetes mellitus, hypertension, smoking, hyperlipidemia, hypercholesterolemia and coronary artery disease. Therefore, no comparisons were made between and within groups for predisposing diseases. Even though excluding patients with low testosterone levels have led to more homogenic patient cohort, relying on single testosterone measurement would have resulted in excluding some patients with normal gonadotropic axis.19 However, our patient number is reasonable even after such exclusion.
A significant short-coming of our study was lack of standardization of penile Doppler scans as well as reporting of the gray-scale findings such as anatomical variations of the penile vascular system. This was due to high diversity of the ultrasound-performers in the routine practice and is a result of retrospective fashion of the study.
ConclusionsPsychogenic ED prevalence is significantly higher in patients who are under 40 years of age respective to the elders. However, psychogenic ED comprises most of the admissions in both the younger and the elder patients.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingNone declared.
Conflicts of interestThe authors have no potential conflicts of interest to disclose.