Effective communication and interpersonal skills among medical emergency staff enhance service quality, reduce errors, boost patient satisfaction, and decrease stress. Role-playing and team-based learning are key methods to improve these skills, but determining the most effective approach is challenging. This study aimed to compare the impact of these 2 methods on the interpersonal communication skills of medical emergency staff at Abadan University of Medical Sciences in 2024.
Material and methodsThis study used a semi-experimental pre-test–post-test design, targeting medical emergency staff at Abadan University of Medical Sciences in 2024. Sixty-eight eligible staff members were chosen through convenience sampling and assigned to 2 groups: role-playing and team-based learning. Data collection involved a demographic form and Wheeless et al.'s interpersonal communication skills questionnaire. Analysis was performed using SPSS version 22, with a significance level established at P < .05.
ResultsThe 2 groups had similar demographic characteristics (P > .05). Before the intervention, the mean score for interpersonal communication skills was 15.46 ± 93.97 in the team-based learning group and 14.30 ± 94.76 in the role-playing group, with no significant difference (P = .82). Post-intervention scores improved to 119.38 ± 11.96 for team-based learning and 131.76 ± 10.51 for role-playing, showing significant improvement, especially in the role-playing group (P = .001).
ConclusionThe study shows role-playing and team-based learning enhance medical emergency staff's communication skills, with role-playing being more effective. Both methods are recommended, emphasizing role-playing for skill enhancement.
La comunicación efectiva y las habilidades interpersonales entre el personal médico de emergencias mejoran la calidad del servicio, reducen errores, aumentan la satisfacción del paciente y disminuyen el estrés. El juego de roles y el aprendizaje basado en equipos son métodos clave para mejorar estas habilidades, pero determinar el enfoque más efectivo es un desafío. Este estudio tuvo como objetivo comparar el impacto de estos dos métodos en las habilidades de comunicación interpersonal del personal médico de emergencias de la Universidad de Ciencias Médicas de Abadan en 2024.
Materials y MétodosEste estudio utilizó un diseño semi-experimental pre-prueba y post-prueba, dirigido al personal médico de emergencias de la Universidad de Ciencias Médicas de Abadan en 2024. Se eligieron sesenta y ocho miembros del personal elegibles mediante muestreo por conveniencia y se asignaron a dos grupos: juego de roles y aprendizaje basado en equipos. La recopilación de datos involucró un formulario demográfico y el cuestionario de habilidades de comunicación interpersonal de Wheeless et al. El análisis se realizó utilizando SPSS versión 22, con un nivel de significancia establecido en p < 0.05.
ResultadosLos dos grupos tuvieron características demográficas similares (p > 0.05). Antes de la intervención, la puntuación media de las habilidades de comunicación interpersonal fue de 15.46 ± 93.97 en el grupo de aprendizaje basado en equipos y de 14.30 ± 94.76 en el grupo de juego de roles, sin diferencia significativa (p = 0.82). Las puntuaciones post-intervención mejoraron a 119.38 ± 11.96 para el aprendizaje basado en equipos y 131.76 ± 10.51 para el juego de roles, mostrando una mejora significativa, especialmente en el grupo de juego de roles (p = 0.001).
ConclusiónEl estudio muestra que el juego de roles y el aprendizaje basado en equipos mejoran las habilidades de comunicación del personal médico de emergencias, siendo el juego de roles más efectivo. Se recomiendan ambos métodos, enfatizando el juego de roles para la mejora de habilidades.
Communication skills are behaviors and actions that allow individuals to interact effectively with others, eliciting positive responses and avoiding negative reactions. These skills enable individuals to establish effective communication, thereby positively influencing others.1
Effective communication is essential for social interaction and is seen by many experts as key to human development and societal progress. Interpersonal communication skills encompass verbal and non-verbal expression, active listening, message interpretation, clarification, questioning, and feedback.2 In education, communication fosters mutual understanding between teachers and students regarding knowledge, culture, and values. In nursing care, effective communication is vital for educating patients about their conditions and treatments and for building therapeutic relationships based on empathy and support, which can enhance patient recovery.3
Enhancing interpersonal communication skills can improve assessment methods for identifying the educational needs of medical emergency professionals, benefiting training programs. Strong communication skills in health sciences are essential, with several educational interventions recommended.4 Active learning fosters lasting attitude changes, while the right teaching methods can make nursing education more engaging and effective. Nurses prefer interactive, real-world approaches, as learning leads to behavioral change and better long-term performance. Choosing suitable teaching methods is crucial for effective training programs, and adopting diverse approaches like lectures, group training, and e-learning can promote enduring learning and increased interest.5
Role-playing is an effective educational technique that fosters active learning and experiential understanding. By engaging learners in discussion, problem-solving, and creativity, it enhances their skills. Training in realistic environments improves skill acquisition, and role-playing offers advantages such as reduced training time and costs, enhanced performance, better decision-making, improved critical-thinking, and increased communication skills. This method is applicable at all education levels and is particularly useful for teaching communication skills through repetition, observation, discussion, and real-life simulations, aligning well with other educational programs.6
Team-based learning (TBL) is a collaborative educational method used since the 1970s, particularly in health-related fields. It promotes active participation and can be implemented by a single instructor in large classes without the need for specific small group spaces. TBL enhances communication skills, builds confidence, and encourages constructive discussions and critical-thinking.7 It fosters a supportive environment where students can express opinions and engage in meaningful dialog. Additionally, small group learning further improves problem-solving and interpersonal skills by increasing learner interaction and motivation. Overall, TBL emphasizes individual and team accountability, aiming to enhance cognitive learning through collaboration.8
Research indicates that the impact of role-playing and TBL on interpersonal communication skills might be understated, as findings from such studies can hold significant implications for emergency medical personnel. Hence, the objective of this study is to compare the effects of training through role-playing and TBL on the interpersonal communication skills of emergency medical staff at Abadan University of Medical Sciences in the year 1403.
Materials and methodsStudy designThe present study is a semi-experimental research designed with a pre- and post-test framework. In this research, the target population consisted of the staff of emergency medical services in Abadan, Khorramshahr, and Shadegan, affiliated with Abadan University of Medical Sciences in the year 2024.
ParticipantsThe research environment was focused on the emergency medical service centers of Abadan University of Medical Sciences.
The inclusion criteria for the research mandate that participants must willingly sign an informed consent form, possess a minimum of 1 year of work experience, hold at least an associate's degree, and have no speech, hearing, or visual impairments. Conversely, individuals will be excluded from the study if they choose to withdraw from participation, utilize other resources, content, or educational methods during the research period, or engage in information exchange between groups through self-reporting.
SamplingThis research was conducted in a semi-experimental and comparative manner using a pre- and post-test design, aimed at comparing the effects of 2 training methods—role-playing and TBL—on the interpersonal communication skills of emergency medical personnel at Abadan University of Medical Sciences. The statistical population of this study consisted of all emergency medical personnel (from Abadan, Khorramshahr, and Shadgan) at Abadan University of Medical Sciences in the year 2024.
The total study population comprised 182 individuals, of whom 121 were deemed eligible for participation. Fifty-three individuals were excluded for various reasons, including a lack of willingness to participate. As a result, 68 participants remained. These individuals were then randomly assigned to 2 distinct groups using a simple randomization method, specifically a coin toss (Fig. 1).
Data collectionThe data collection tools used in the current research are as follows.
Demographic characteristics formThis form includes information about age, gender, marital status, education level, work experience, number of children, spouse's occupation, workplace, and financial status.
Interpersonal communication skills questionnaire by Vakili and colleaguesThe interpersonal communication skills questionnaire developed by Vakili and colleagues consists of 7 scales, each containing 6 questions.9 This questionnaire uses a 5-point Likert scale for responses, with the scoring system categorized as follows: very poor (scores 1–4), poor (scores 5–8), average (scores 9–12), good (scores 13–16), and excellent (scores 17–20). The scales covered in this questionnaire are:
- •
General communication skills.
- •
Speaking communication skills.
- •
Active listening communication skills.
- •
Interpretation and clarification skills.
- •
Questioning skills.
- •
Feedback skills.
- •
Encouragement and praise skills.
- •
The validity and reliability of this tool have been assessed and confirmed by Vakili and colleagues.
The total score for interpersonal communication skills for each individual ranges from a minimum of 37 to a maximum of 185. The operational definition of overall interpersonal communication skills is outlined as follows:
- •
Weak overall interpersonal communication skills: scores between 37 and 69.
- •
Average overall interpersonal communication skills: scores between 70 and 109.
- •
Good overall interpersonal communication skills: scores between 110 and 149.
- •
Excellent overall interpersonal communication skills: scores between 150 and 185.
The validity of this questionnaire was calculated based on the content validity assessed by Vakili and colleagues, where the values for all items were above 0.7. The reliability of the questionnaire was calculated using Cronbach's alpha, resulting in the following: general communication skills scored 0.85, speaking communication skills scored 0.83, listening communication skills scored 0.80, interpretation and clarification skills scored 0.80, questioning skills scored 0.74, feedback skills scored 0.77, and encouragement and praise skills scored 0.79. Based on the results from this research, the overall Cronbach's alpha for the interpersonal communication skills questionnaire was found to be 0.88.
InterventionThe present study was a quasi-experimental study employing a pre- and post-test design. The statistical population consisted of all personnel from the Medical Emergency Services in Abadan, Khorramshahr, and Shadgan affiliated with Abadan University of Medical Sciences in the year 2024. Initially, after the research proposal was approved by the Research Council of Alborz University of Medical Sciences and received ethical approval from the University's Ethics Committee with the identification number (IR.ABZUMS.REC.1403.031), and after obtaining an official letter of introduction from the esteemed Research Vice President of the University, the researcher presented this introduction and explained the research objectives to the heads of the research environments to gain their consent and cooperation. Subsequently, the researcher visited the specified departments and selected personnel from the medical emergency services in Abadan, Khorramshahr, and Shadgan who met the inclusion criteria for the study. After discussing the study's objectives with the participants, they were invited to participate in the study. Individuals who met the inclusion criteria and were willing to participate signed a written informed consent form after reviewing the information and entered the research.
Team A: Initially, the role-playing team conducted a pre-test, followed by a 5-h educational session. The post-test was conducted 1 week later.
Team B: Initially, the team engaged in TBL, followed by a 5-h educational session, with the post-test occurring 1 week later.
Team-based learning methodIn this study, 2 methods were utilized for training participants: role-playing and TBL. The TBL method was implemented in the educational class at the Medical Emergency Services Center of Abadan University of Medical Sciences as follows:
- (1)
Preparation: Initially, arrangements were made with the participants regarding the time and date of the TBL session, which took place during working hours, in-person, lasting 5 h, and was conducted by the project implementer. The topics covered included definitions of basic communication terms and concepts, types of communication, interpersonal communication types, essential steps for establishing effective communication, stages of communication, selecting the type of message appeal, executing a communication process, verbal communication skills, methods used to enhance interpersonal communication, different communication personality types, health communication, the definition of educational media in health, the educational media's role in promoting health, and the eight influential factors on the efficacy of educational media content.
- (2)
Individual readiness assessment (IRAT): Following class activities, a 4-option multiple-choice test prepared from the relevant content was conducted. The questions were derived from key topics that prompted group discussions among team members, during which 10 multiple-choice questions were formulated.
- (3)
Team readiness assessment (TRAT): Immediately after the individual test, the same test was administered in a group format. Both individual and team assessments were executed to ensure participant engagement.
- (4)
Study (APPEALS): In this phase, group members could refer to the material they had previously studied and justify their answers while defending their responses. After completing the test, team members filled out a reconsideration form for questions they answered incorrectly in the team assessment stage.
- (5)
Feedback: From team members present in the session.
- (6)
Group assignment (TAP): The most critical aspect in designing assignments for TBL was ensuring that these tasks fostered interaction within the group, thus obliging the learners to make decisions and report on the choices made.10
Individual and team tests were administered after class activities. In this stage, a total of 10 multiple-choice questions related to the specified content were given to the personnel, who were requested to answer them individually and without reference materials within a set time (averaging 7 min). After the allotted time, the team leader was asked to collect and submit the individual answer sheets. The same test was then conducted within the team, where team members discussed each question and selected a consensus answer to submit as their team's response. This process took, on average, 12 min. After collecting the group answer sheets, the instructor read each question in the class and asked each group to explain their collective reasoning for the selected answers. For questions requiring further clarification, detailed explanations were provided, leading to the determination of scores for each team. Subsequent to this, personnel were given the opportunity to contest the answer key or question wording and follow this up with a written objection on a reconsideration form. This form, designed by the researcher, allowed staff to note the question in question and provide reasons along with references for their objection. This step could occur post-class. Rebuttals must be compiled in writing and as a team. If the team's objections were validated, the team score would be adjusted accordingly.
Role-playing methodStage 1: Topic selection.
Initially, participants were asked to coordinate on the timing and date of the session. The class convened during working hours for a 5-h in-person format. Identifying and selecting a topic is the first step in the role-play model, which can be derived from either the lesson topic (subject matter taught) or topics selected by participants based on their interests. During this phase, the following criteria must be adhered to:
- (1)
The topic must be clear and understandable.
- (2)
The topic must be of general interest and agreement among participants.
- (3)
The topic should have significant social goals.
- (4)
The topic must be feasible and amenable to discussion within the role-play framework.
- (5)
The topic should be engaging and suitable for the mental and psychological capabilities of participants. In this method, all individuals have roles and must act accordingly within set timelines, actively participating in the learning process.
Stage 2: Script writing.
The script encompasses the primary structure of the role-play model. At this stage, all activities from start to finish are written in a conversational style. The fundamental goals of the instructional content should be included in each step. Social values must be upheld, avoiding undesirable habits and inappropriate content. Participants should implement executable strategies in subsequent stages. At this step, consideration must be given to the participants' capabilities and their intellectual backgrounds, which are crucially important. The script should have a clear beginning and conclusion, providing necessary training content. If the desired script is poorly structured, it will diminish participants' motivation to perform, and the presentation may lack intended appeal.
Stage 3: Role assignment.
Selecting actors based on their abilities and interests in the desired roles is the most critical part of the role-play model. The number of roles, selection of individuals, and other execution matters must be taken into consideration. Recognizing individuals' personalities and behavioral traits, as well as physical characteristics (height, weight, age, etc.), is highly significant. The instructor, acting as the director, should get to know their capacities beforehand and recommend roles accordingly. The opinions of other participants and observers should also play a role in this selection.
Stage 4: Provision of required resources and equipment.
Based on the developed script, the necessary resources should be identified and gathered. The role of these materials in shaping and strengthening the execution process and the effectiveness of the script is crucial, especially for the participants, as it renders the experience engaging and compelling. Creating an environment, appropriately setting the stage, and assembling additional materials or resources is essential, along with clearly demonstrating their use to the actors. Preferably, simple and accessible materials should be utilized, with participants themselves creating the stage props when possible.
Stage 5: Preparation and preliminary rehearsal.
After determining roles and outlining tasks, preparations must be undertaken. Under the guidance of the instructor, the actors should rehearse initial actions. These preparations include:
- (1)
Memorizing their respective roles.
- (2)
Carefully studying the entire script to understand the roles of others.
- (3)
If needed, knowing faces and applying makeup to depict characters.
- (4)
Identifying and preparing necessary materials and resources.
- (5)
Recognizing the execution phases and rehearsing them sequentially.
Stage 6: Script execution.
In this phase, in the presence of other participants and the instructor, the group of actors performs their respective roles. The instructor's presence as the guiding director is vital for this phase. The execution of the role-play model and the performance of the script in class is the main focus. In this phase, observers should attentively watch the execution while remaining orderly and are encouraged to take note of important points and suggestions for improvement if possible. It is noteworthy that other goals and expectations must be reflected in the behavior and speech of the actors. Additionally, attention must be paid to ensure that the execution process does not overshadow the goals, and the method of performing the tasks remains aligned with the intended outcomes.
Stage 7: Discussion, review, and evaluation.
After the performance phase concludes, observers participate in a group evaluation of all stages of execution led by the instructor, where they offer their critiques and suggestions. The goal of this phase is to amend and enhance the positive aspects while addressing any negative elements in the script and role performances. All insights must be considered in subsequent decisions. These suggestions hold significant weight for the instructor, who directs the performance, as adhering to them can enhance the effectiveness of the method. At this stage, reviewing and analyzing the distribution of the script and the execution process for participants must also be carried out.11
Training sessions were conducted during official hours under the supervision and coordination of the education officer of the Emergency Services Center, organizing two 5-h training sessions for the role-playing teams and the TBL method.
Statistical analysisFor data analysis, SPSS software version 21 was used. Initially, descriptive statistics such as statistical tables, charts, and indicators of mean, standard deviation, frequency, and percentage were employed to describe the data. Subsequently, inferential statistics were utilized through tests such as Fisher's exact test, chi-square test, independent t-test, and paired t-test.
ResultsDemographic characteristicsAccording to Table 1, the mean age of the personnel in the TBL group was 34.20 years, with a standard deviation of ±7.70 years. In contrast, the mean age in the role-playing group was 32.67 years, with a standard deviation of ±6.13 years. An independent t-test revealed that there was no statistically significant difference in mean age between the 2 groups (P = .36).
Demographic Information.
| Variable | Category | Team-based learning team | Role-playing team | ||
|---|---|---|---|---|---|
| N | Percentage | N | Percentage | ||
| Age (Year) | 20–30 | 14 | 41.2 | 18 | 52.9 |
| 31–40 | 14 | 41.2 | 12 | 35.3 | |
| Above 40 | 6 | 17.6 | 4 | 11.8 | |
| Mean ± Standard deviation | 34.20 ± 7.70 | 32.67 ± 6.13 | |||
| t-test results | t = 0.90 df = 66 P = 0.36 | ||||
| Marriage status | Single | 4 | 11.8 | 6 | 17.6 |
| Married | 30 | 88.2 | 28 | 82.4 | |
| Fisher test results | X2 = 0.46 df = 1 P = 0.73 | ||||
| Level of education | Associate degree | 26 | 76.5 | 26 | 76.5 |
| Bachelor | 8 | 23.5 | 8 | 23.5 | |
| Fisher test results | X2 = 0.00 df = 1 P = 1 | ||||
| Number of children | 0 | 7 | 20.6 | 10 | 29.4 |
| 1 | 10 | 29.4 | 11 | 32.4 | |
| 2 | 8 | 23.5 | 9 | 26.5 | |
| 3 | 5 | 14.7 | 2 | 5.9 | |
| 4 | 4 | 11.8 | 2 | 5.9 | |
| Fisher test results | X2 = 2.58 df = 4 P = 0.67 | ||||
| Financial status | Weak | 4 | 11.8 | 7 | 20.6 |
| Average | 20 | 58.8 | 21 | 61.8 | |
| Good | 10 | 29.4 | 6 | 17.6 | |
| Chi-square test results | X2 = 1.84 df = 2 P = 0.38 | ||||
| Spouse's occupation | Self-employed | 5 | 14.7 | 6 | 17.6 |
| Housekeeper | 18 | 52.9 | 19 | 55.9 | |
| Employee | 11 | 32.4 | 9 | 26.5 | |
| Chi-square test results | X2 = 0.31 df = 1 P = 0.89 | ||||
| Housing | Owned | 19 | 55.9 | 17 | 50 |
| Rental | 15 | 44.1 | 17 | 50 | |
| Fisher test results | X2 = 0.23 df = 1 P = 0.80 | ||||
| Work experience (Years) | 2–6 | 10 | 29.4 | 21 | 61.8 |
| 7–12 | 15 | 44.1 | 9 | 26.5 | |
| More than 12 | 9 | 26.5 | 4 | 11.8 | |
| Mean ± Standard deviation | 4.90 ±7.44 | 5.68 ±9.97 | |||
| t-test results | t = 1.96 df = 66 P = 0.054 | ||||
The majority of emergency medical personnel in both the TBL group (88.2%) and the role-playing group (82.4%) were married. Fisher's exact test indicated that there was no statistically significant difference in marital status between the 2 groups (P = .73).
A significant portion of the emergency medical personnel held an associate degree, with 76.5% of the TBL group and the role-playing group possessing this level of education. Fisher's exact test demonstrated that there was no statistically significant difference in educational levels between the 2 groups, suggesting they were completely homogeneous (P = 1).
A notable percentage of emergency medical personnel in both the TBL group (29.4%) and the role-playing group (32.4%) were only children. Fisher's exact test indicated that there was no statistically significant difference between the 2 groups in terms of the number of children (P = .67).
The majority of emergency medical personnel in both groups exhibited an average financial status, with 58.8% in the TBL group and 61.8% in the role-playing group falling into this category. The chi-square test revealed that there was no statistically significant difference between the 2 groups regarding their financial status (P = .38).
The spouses of most emergency medical personnel were homemakers, with 52.9% in the TBL group and 55.9% in the role-playing group. The chi-square test indicated that there was no statistically significant difference between the 2 groups regarding the occupation of their spouses (P = .89).
The majority of personnel in the medical emergency team utilizing a TBL approach (55.9%) owned personal housing. Similarly, half of the personnel in the role-playing group (50%) owned personal housing, while the other half did not. Fisher's exact test showed that there was no statistically significant difference in housing status between the 2 groups (P = .80).
The average work experience among the personnel in the TBL group in emergency medical services was 9.97 ± 5.68 years, compared to 7.44 ± 4.90 years in the role-playing group. An independent t-test indicated that there was no statistically significant difference in average work experience between the 2 groups (P = .54).
Interpersonal communication skills scores and its dimensions before and after the interventionAs shown in Table 2, the mean and standard deviation of interpersonal communication skills scores among emergency medical personnel before the intervention were 46.15 ± 93.97 in the TBL group and 30.14 ± 94.76 in the role-playing group. An independent t-test revealed no statistically significant difference between the 2 groups (P = .82). Post-intervention, the mean and standard deviation of interpersonal communication skills in the team-based learning group increased to 11.96 ± 119.38, while in the role-playing group, they reached 10.51 ± 131.76. The independent t-test indicated that this difference was significant, suggesting an improvement in interpersonal communication skills among emergency medical personnel in the role-playing group (P = .001). A comparison of the mean scores and standard deviations of interpersonal communication skills among emergency medical personnel before and after the intervention in the TBL group, using the paired t-test, revealed a significant difference from pre- to post-test (P < .001). Similarly, in the role-playing group, the difference from pre- to post-test was also significant (P < .001).
Mean and standard deviation of the score of interpersonal communication skills and its dimensions in emergency medical personnel before and after the intervention.
| VariableGroup | Before intervention | After intervention | Paired t test results | |||||
|---|---|---|---|---|---|---|---|---|
| Mean | Standard deviation | Mean | Standard deviation | |||||
| Public communication skills | TBL | 19.35 | 3.54 | 25.11 | 2.85 | 001. > P | df = 33 | t = −8.08 |
| RP | 20.79 | 3.06 | 27.61 | 2.13 | 001. > P | df = 33 | t = −12.09 | |
| Independent t-test results | t = −1.79 df = 66 P = .07 | t = −4.08 df = 66 P < .001 | ||||||
| Speaking communication skills | TBL | 12.94 | 2.36 | 16.50 | 1.84 | P < .001 | df = 33 | t = −8.29 |
| RP | 14.2 | 2.90 | 17.76 | 1.85 | P < .001 | df = 33 | t = −8.58 | |
| Independent t-test results | t = −1.69 df = 66 P = .09 | t = −2.81 df = 66 P = .006 | ||||||
| Active listening communication skills | TBL | 12.79 | 2.48 | 16.73 | 1.86 | P < .001 | df = 33 | t = −7.52 |
| RP | 12.70 | 2.48 | 18.14 | 1.74 | P < .001 | df = 33 | t = −11.08 | |
| Independent t-test results | t = 0.14 df = 66 P = .88 | t = −3.22 df = 66 P = .002 | ||||||
| Interpreting and clarifying the audience's speech | TBL | 12.44 | 2.58 | 12.61 | 2.77 | P < .001 | df = 33 | t = 0.29 |
| RP | 12.32 | 3.22 | 15.23 | 2.68 | P < .001 | df = 33 | t = 44/4- | |
| Independent t-test results | t = 0.16 df = 66 P = .86 | t = −3.95 df = 66 P < .001 | ||||||
| Communication skills of asking questions | TBL | 12.05 | 2.38 | 16.14 | 2.27 | P < .001 | df = 33 | t = −9.47 |
| RP | 12.00 | 2.87 | 17.47 | 2.28 | P < .001 | df = 33 | t = −9.04 | |
| Independent t-test results | t = 0.09 df = 66 P = .92 | t = −2.39 df = 66 P = 0.01 | ||||||
| Feedback communication skills | TBL | 11.97 | 2.51 | 16.38 | 2.25 | P < .001 | df = 33 | t = −8.73 |
| RP | 11.32 | 2.72 | 17.38 | 2.14 | P < .001 | df = 33 | t = −11.10 | |
| Independent t-test results | t = 1.01 df = 66 P = .31 | t = −1.87 df = 66 P = .06 | ||||||
| Communication skills of encouragement and praise | TBL | 12.41 | 2.90 | 15.88 | 2.72 | P < .001 | df = 33 | t = −5.15 |
| RP | 11.58 | 3.40 | 18.14 | 1.51 | P < .001 | df = 33 | t = −10.08 | |
| Independent t-test results | t = 1.07 df = 66 P = .28 | t = −4.19 df = 66 P < .001 | ||||||
| Total interpersonal communication skills | TBL | 93.97 | 15.46 | 119.38 | 11.96 | P < .001 | df = 33 | t = −8.62 |
| RP | 94.76 | 14.30 | 131.76 | 10.51 | P < .001 | df = 33 | t = −14.59 | |
| Independent t-test results | t = −0.22 df = 66 P = .82 | t = −4.53 df = 66 P = .001 | ||||||
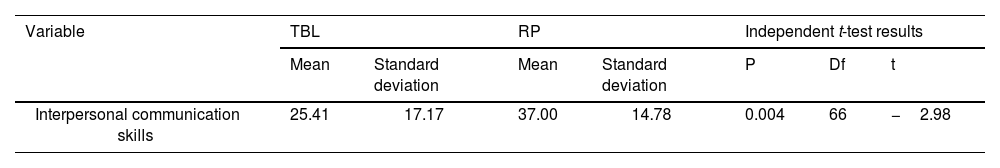
According to Table 3 and Fig. 2, the independent t-test showed that the mean change in interpersonal communication skills scores in the role-playing group was significantly higher than that in the TBL group (P = .004).
This study aimed to “compare the effects of 2 educational methods—role-playing and TBL—on the interpersonal communication skills of emergency medical personnel at Abadan University of Medical Sciences in 2024.”
The average scores of interpersonal communication skills in the studied samples before and after training using the role-playing methodBased on the findings, the average scores of interpersonal communication skills among emergency medical personnel in the training group using the role-playing method improved from the pre-test to the post-test. This finding indicates the effectiveness of the role-playing training method on the interpersonal communication skills of emergency medical personnel. This means that the role-playing method can be used to enhance the interpersonal communication skills of emergency medical personnel.
In this context, a study by Dary and colleagues (2020), titled “Comparing two methods of role-playing and conventional education on the long-term learning of nursing students,” concluded that role-playing training is effective for long-term learning in nursing students.12 Additionally, a study by Sepahvandi et al. (2019) titled “Examining the impact of storytelling through role-playing on the communication and social skills of children with autism” demonstrated that storytelling through role-playing is an effective and cost-efficient therapeutic intervention for improving the communicative and social performance of children with autism.13
Furthermore, Larti et al. (2018) conducted a semi-experimental study titled “Investigating the impact of a role-playing educational program centered on empathy with the patient on the communication skills scores of operating room students.” The findings indicated that teaching empathetic communication through role-playing enhances the communication skills scores of the students in this field. Role-playing emerged as an engaging teaching method for students, suggesting the need for curriculum modifications to familiarize operating room students with essential communication skills.14
Karabasi and colleagues (2018) aimed to “determine the impact of teaching communication skills with patients through role-playing on the self-efficacy of nursing students,” finding that implementing role-playing techniques compared to traditional methods significantly enhances the self-efficacy of undergraduate nursing students.15 Ferd and colleagues (2019) evaluated the impact of role-playing training on splinting skills in nursing and emergency medical students, concluding that role-playing was effective in enhancing splinting skills.16
The researcher believes that the main reason for the alignment of these studies and their similar outcomes relates to the nature of education. Presenting information on a specific topic, irrespective of the method, enhances learners' knowledge and awareness. Role-playing serves as an effective learning technique as it compels individuals to consider the perspectives of the characters they portray. This teaching model addresses issues through practice at its core and is rooted in individual and social dimensions of education.
However, differences with the previously examined studies may arise from variations in target groups, intervention content, the number and duration of sessions, as well as the timing and context of the research.
Average scores for interpersonal communication skills before and after team-based learningAccording to the findings, the average scores for interpersonal communication skills among emergency medical personnel in the TBL training group improved from the pre-test to the post-test. This demonstrates the effectiveness of the TBL educational method in enhancing the interpersonal communication skills of emergency medical personnel. Therefore, TBL can also be utilized to improve these communication skills.
In this regard, a study conducted by Ghiyasvandian et al. (2021), titled “Investigating the effects of team-based learning on the learning and academic motivation of emergency medicine students in the triage course,” concluded that employing the TBL method increases motivation and improves learning in emergency medicine students.17
Persky and colleagues (2012) assessed the impact of team-based education on a basic pharmacokinetics course for pharmacy students at the Eshelman School of Pharmacy in North Carolina, USA. The results indicated that by the end of the TBL course, students' assessment scores (learning) significantly improved compared to the previous year, and specialized scores showed a consistently upward trend. At the end of the term, students' attitudes, skills, and active engagement demonstrated significant improvement.18 In a study by Jabbar et al. (2018), aimed at assessing the effectiveness of TBL strategies on the performance of medical students at the University of Sharjah in the United Arab Emirates, 112 students were invited, and ultimately 100 (64 female and 36 male) completed the survey and were tested. The results showed no significant difference in resources used in classes, but there was a significant correlation between students' performance in the TBL course and their final exam scores. Overall, students' attitudes toward the TBL system were described as positive and encouraging.19
The findings from the study by Imamian Kheshti et al. (2016), titled “The impact of integrating Merrill's principles of instruction and team-based learning on recall and application in nursing students,” revealed that the experimental group achieved significantly better results in recall and application compared to the control group. Consequently, the integration of Merrill's principles with TBL can enhance achievement levels in terms of recall and application.20
In this case, the researcher believes that the primary reason for the similarity in studies and the acquisition of similar results is also related to the educational methods employed. Presenting information on a specific topic through TBL can enhance learners' knowledge and awareness. TBL is a new form of collaborative learning that creates an active and participatory learning environment, without the need for dedicated small group spaces or increased instructor numbers; it can effectively be implemented with one instructor in a large classroom. The goal of this approach is to enhance learners' skills in achieving higher cognitive learning levels through the application of personal knowledge within a team setting, often referred to as collaborative learning.21 However, differences from the previously examined studies include variations in target groups, intervention content, the number and duration of sessions, as well as the timing and context of the research. In this current study, the researcher chose emergency medical personnel as the target group, with a focus on enhancing interpersonal communication skills, which differs from triage and pharmacy disciplines, as well as students in the United States and the UAE.
Comparison of interpersonal communication skills scores between role-playing and team-based learningBased on the findings, after the study, the average scores for interpersonal communication skills among emergency medical personnel in both the TBL and role-playing groups improved from the pre-test to the post-test. However, the average scores in the role-playing group were significantly higher than in the TBL group. This finding suggests that for enhancing interpersonal communication skills among emergency medical personnel, role-playing is the preferred method.
In this context, a study by Dary et al. (2020) titled “Comparing two educational methods—role-playing and conventional training—on long-term learning in nursing students” found that role-playing training was more effective than other methods.12 Although both this study and the one by Dary et al. identified role-playing as the more effective method, the current study specifically compared role-playing with TBL, which differs from conventional training methods. The aim of this study was focused on enhancing interpersonal communication skills, unlike the long-term learning outcomes explored in nursing education.
However, contrary to the results of the current study, a study by Khodizadeh et al. demonstrated that both role-playing and video feedback methods had equivalently positive impacts on midwives' communication behaviors with parturients.22 The discrepancies between this study and that of Khodizadeh et al. can be attributed to differences in target populations, intervention content, the number and timing of sessions, as well as study environment and timing.
At times, studies have shown distinct findings where TBL proved more effective. For instance, Shar'ee Malashahi et al. (2019) conducted a study comparing the effects of 2 teaching methods—TBL and classical lecturing—on knowledge and attitudes among midwifery students in obstetric emergencies, with results indicating a significant difference between the mean scores from the lecture and TBL methodologies. The findings also indicated a positive attitude from students following TBL instruction in obstetric emergencies.21 Additionally, Hosseini and colleagues compared the 2 methods of “role-playing” and “bedside training” in patient handling and transfer among physical therapy students, concluding no significant difference between the efficacy of the 2 groups in enhancing skills for transferring patients with spinal injuries.23
Various factors could have influenced these findings, such as prior preparation and study before teaching, repeated assessments conducted during sessions, the effects of group interaction, lecturer feedback, and the students' engagement with case studies in the TBL process.
LimitationA: Limitations within the researcher's control: Certain psychological states, such as fatigue, anxiety, work pressure, and impatience, could have influenced the responses of the study participants while filling out the questionnaires. To mitigate this limitation, measures were taken to create an appropriate environment and ample time for completion of the questionnaires. Moreover, the researcher made follow-up visits at more suitable times to provide support and address any potential ambiguities.
B: Limitations beyond the researcher's control: Individual, social, and cultural differences among the participants may have affected their understanding and response styles, and these variations are beyond the researcher's control. Additionally, there was a possibility of information exchange between the 2 groups, which was also outside the researcher's jurisdiction.
RecommendationsThe findings indicate that 2 training methods—role-playing and TBL—are effective in enhancing the interpersonal communication skills of emergency medical personnel. However, the role-playing method has been found to be more effective than the other. Therefore, it is recommended that both methods, particularly the role-playing approach, be employed to improve the interpersonal communication skills of emergency medical personnel.
At the conclusion of the conducted studies, it is essential to present suggestions for future research based on the strengths and weaknesses identified. These recommendations, stemming from the researcher's efforts and experiences throughout different stages of the investigation, could serve as a foundation for further studies that complement and extend the current research. In light of the experiences gained during this study, the following suggestions are proposed for future research:
- (1)
Compare the impact of role-playing and TBL methods on the interpersonal communication skills of emergency medical personnel from the perspective of patients.
- (2)
Compare the effects of role-playing and TBL methods on the triage skills of emergency medical personnel at Abadan University of Medical Sciences.
The research was approved by the Research Council of Alborz University of Medical Sciences and received ethical approval from the University's Ethics Committee with the identification number (IR.ABZUMS.REC.1403.031). The ethics committee's approval and the informed consent of the participants were essential components of the research, ensuring that the study was conducted ethically and responsibly.
The authors declare that they have no conflicts of interest.