Simulations make it possible to acquire various skills in a risk-free environment. The objective of this study was to assess medical students¿ performance in a simulation-enriched learning scenario in renal disease.
Methods2 renal scenarios were designed for implementation in high-fidelity simulations, using a rubric to assess small student teams’ performance. Good Judgment Debriefing was used as feedback to the students, once the simulation had ended. Finally, students then completed a self-evaluation of their performance.
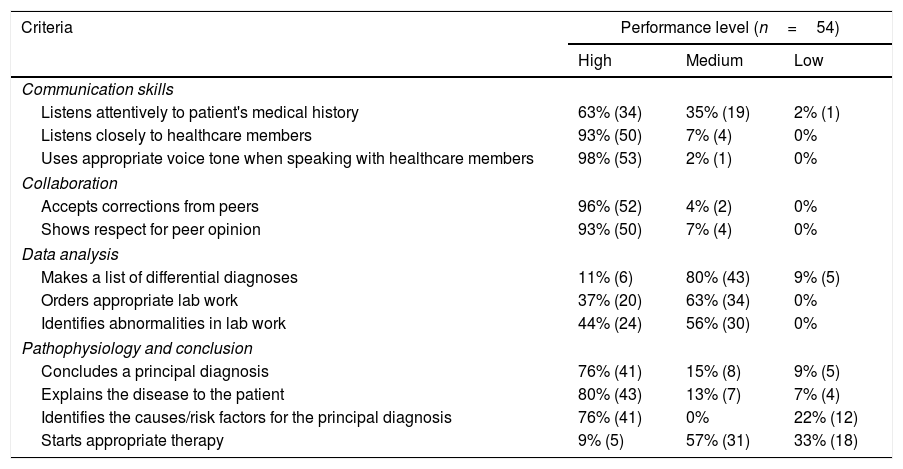
Results54 students voluntarily participated in this study. Student teams performed the best in communication, collaboration and understanding of pathophysiology skills.
ConclusionsCommunication skills are of great importance in the medical field, both with healthcare team as with the patient. Students must strengthen their performance in therapy implementation and differential diagnoses before entering clinical rotations. This activity allows deep reflection and analysis of specific area performance, which can augment confidence on those where performance is high; and identify weakness areas that will lead to designing new activities to strengthen them.
La simulación permite adquirir diversas habilidades sin correr riesgos. El objetivo del estudio es evaluar el desempeño de los estudiantes de medicina dentro de un escenario de aprendizaje de enfermedades renales enriquecida con simulación.
MétodosSe diseñaron 2 escenarios de enfermedades renales para simulaciones de alta fidelidad, usándose una rúbrica de desempeño para evaluar los equipos pequeños de alumnos. La retroalimentación se dio mediante debriefing con Buen Juicio. Finalmente, los alumnos realizaron una auto-evaluación de su desempeño.
ResultadosLos puntajes más altos se obtuvieron en comunicación, colaboración y entendimiento de la fisiopatología.
ConclusionesLas competencias de comunicación con el paciente y el personal de salud son de gran importancia en el campo médico. Los alumnos deben mejorar su desempeño en implementar tratamiento y diagnóstico diferencial antes de entrar a sus rotaciones clínicas. Esta actividad permite una reflexión profunda y análisis del desempeño en áreas específicas, lo que puede favorecer la confianza en las áreas con alto desempeño e identificar áreas de oportunidad.
Worldwide medical schools have had great interest in providing learning environments from which their students can achieve skills intended to provide high quality medical attention to their patients upon graduation. During the first years of medical school, students receive a variety of theoretical courses whose information sometimes is difficult to apply in a clinical setting. Some authors mention simulators have been used effectively for learning basic sciences1; where scenarios can significantly engage students by learning in a risk-free environment both for patients and students, strengthening collaborative work.2,3 Several authors1,4 have described simulation practices for undergraduate students, where role-playing, standardized patients, computers, videos and low or high-fidelity mannequins are used. The first two must follow a previously written script. Computers can be used to simulate arrhythmias, pulmonary function abnormalities, etc. Videos can be used to assess self- and non-self experience. Mannequins can help place a student in a specific clinical setting where he can interact in different ways with specific physiologic parameters presented to him; conferring greater recall and satisfaction by students. They must identify the most important variables in a given situation and make clinical decisions for diagnosis, treatment, effective communication with healthcare personnel or the patient, etc. Simulations are an useful and resourceful tool for learning diverse skills in a context very similar to real-life experience.
Some centers have used the mastery learning technique in which the student can repeat a given practice as many times as needed to achieve a given level of competency,5 especially in cardiopulmonary resuscitation (CPR) and advanced vital support; but also in clinical rotations in ObGyn, internal medicine, pediatrics and surgery. In recent years, preclinical training has been using simulation. Complete medical history and physical exam can be addressed in a mannequin or a standardized patient, with great realism, where the student can identify changes in vital signs, cardiac and respiratory sounds, abdominal alterations, pulses, etc.
DebriefingAmong the different techniques available for structured feedback, debriefing has been widely accepted due to the satisfactory results obtained.6 Some authors6–9 describe debriefing as the process in which tutors and students reexamine a clinical situation by reflexive discussion, that allows responding to a clinical situation in a systematic and orderly way; which cam be used in combination with problem based learning (PBL).9 There are different types of debriefing. Good Judgment Debriefing stimulates learning the most in health area students10; and requires the tutor to have an active role in order to be able to understand the mechanisms by which students make decisions for doing or saying, therefore being able to identify areas to be reinforced or changed for better understanding of a specific content or identify actions to be done in a specific clinical situation.
The objective of this study was to assess medical students’ performance in a simulation-enriched learning scenario in renal disease.
MethodsThis activity had two phases: design and implementation. The design phase included planning and design of the simulated experience as well as the creation of the evaluation tools. Two clinical scenarios were designed for simulations for third year medical students related to renal diseases. Both scenarios were designed to be applied to small group of students. The simulator was selected according to the realism required by the designed scenario. The scenario information was downloaded in the simulator by the technician prior to the implementation of the simulation.
In order to objectively assess the students’ performance, an evaluation rubric was designed which included the level of performance of each student in the following criteria: acquisition of medical history, communication with healthcare team, communication with the patient, identification of abnormalities in labs and paraclinical exams, communication of these abnormalities to the patient, explaining the differential diagnosis to the patient, explaining risk factors to the patient, and starting appropriate therapy. Each criteria included specifications for grading, including number of family members included in the family medical history, the number of symptoms asked to the patient, the number of times the medical team shared information about the case (medical history, lab results, variations in vital signs, etc.) among themselves, the number of times the medical team spoke with the patient, type of language used and information explained to the patient.
All participating students were informed of the nature of the investigation and signed a written informed consent prior to participation in the study. In the second phase, implementation of the simulation, students were divided into small groups of three or four students each. After receiving a brief introduction to the clinical setting, students entered an area simulating an emergency room with a high-fidelity mannequin which showed specific vital signs alterations. They could interrogate the patient, ask for labs and paraclinical tests to complete the information necessary to make a diagnosis for the patient and install treatment, and finally explain the situation to the patient. Scenarios were run for approximately 10min. Students were challenged with a patient who comes to the clinic with some of the diseases discussed previously in class. Students should have a diagnosis and explain the mechanisms of the disease to the patient. Implementation took place in the Simulation Center of a private medical school in northern Mexico during the first semester 2016. During the simulation, students were evaluated by the tutor using a specific rubric designed for the scenarios. After the simulation, students participated in a Good Judgment Debriefing session, following the steps described by Maestre and Rudolph.10
Statistical analysisResults54 students voluntarily participated in this study. The majority of the students had had experience with high-fidelity mannequins (60%). They participated in teams in both simulations. The results of the teacher's assessment (Table 1) showed students were able to do a concise interrogation, ask about allergies, meds being taken, chief complaint; but they require to do these in an orderly fashion and systematically. Some teams assigned roles, which favored order in their performance. They were able to do well in communicating information to the patient in lay and understandable language, answering the patient's questions and keeping close eye contact with the patient at all times.
Tutor assessment on student's performance.
| Criteria | Performance level (n=54) | ||
|---|---|---|---|
| High | Medium | Low | |
| Communication skills | |||
| Listens attentively to patient's medical history | 63% (34) | 35% (19) | 2% (1) |
| Listens closely to healthcare members | 93% (50) | 7% (4) | 0% |
| Uses appropriate voice tone when speaking with healthcare members | 98% (53) | 2% (1) | 0% |
| Collaboration | |||
| Accepts corrections from peers | 96% (52) | 4% (2) | 0% |
| Shows respect for peer opinion | 93% (50) | 7% (4) | 0% |
| Data analysis | |||
| Makes a list of differential diagnoses | 11% (6) | 80% (43) | 9% (5) |
| Orders appropriate lab work | 37% (20) | 63% (34) | 0% |
| Identifies abnormalities in lab work | 44% (24) | 56% (30) | 0% |
| Pathophysiology and conclusion | |||
| Concludes a principal diagnosis | 76% (41) | 15% (8) | 9% (5) |
| Explains the disease to the patient | 80% (43) | 13% (7) | 7% (4) |
| Identifies the causes/risk factors for the principal diagnosis | 76% (41) | 0% | 22% (12) |
| Starts appropriate therapy | 9% (5) | 57% (31) | 33% (18) |
As previously mentioned by some authors,1 simulation can be used effectively for teaching basic sciences, as is the present case. In this activity, students are able to apply their theoretical knowledge into a risk-free clinical setting.2,3
The students performed the best on communication skills criteria particularly among the healthcare team. This is an important skill to develop in medical students due to the interaction they will have once they enter clinical rotations, where they will have to communicate with different personnel. The way they react to the opinions of others was well the decisions taken as a team shows the level of maturity in this concept.
Choosing which lab work to perform and understanding the abnormalities present in these had a medium performance. This shows the students knew what to look for, but sometimes were not clear how to order a specific test. They need to be familiar with the most common test used in clinics, as well as the parameters included in each. Some of the students were not familiar with the normal values, but since they listened to peers in team, were able as a whole to overcome this weakness. Also some were able to articulate better all the information obtained.
Listing differential diagnoses had a medium performance. Therapy implementation had a medium performance. Students had had little practice with listing differential diagnoses as well as indicating medication to patients. They sometimes knew what medication to use, but doubted about the dose. This showed an area they need to strengthen before entering clinical rotations. Identifying the principal diagnosis, explaining it to the patient and identifying the principal causes triggering or etiology of the diagnosis had a high performance. Identifying the causes that trigger the diagnosis is of significant importance, since this reflects the understanding of the pathophysiology underlying the diseases discussed in class. In this criteria, students’ performance was on high level, which reflects they have learned the concepts and are able to apply them in a clinical setting, linking them to the patient's vital signs, physical exam, labs abnormalities and response to therapy in the scenario.
This type of activities allows both teachers and students to reflect upon their level of competence in the assessed areas. They can grow in confidence in what they performed highest and can focus on strengthening their weak areas. Teachers can intentionally design activities that can help students in the areas they are having the most trouble with.
From the information obtained in this study, we conclude that the incorporation of simulation in medical education has a positive impact on the development of different types of skills, depending on the simulation design. It reinforces the students’ communication skills, decision-making, critical thinking and the acceptance of responsibility for one's actions as well as for the performance of the medical team. Students become aware of their own capabilities and limitations, by reflecting upon their own performance, the reasons that lead them to making these decisions as well as experiencing the consequences of them in the simulation scenario, as has been mentioned by some authors.7,9,10
We think this kind of activities can be applied to other pathophysiology courses where students learn about different diseases, even if the classical instruction has been predominantly theoretical. Students become engaged in their own learning process and help each other in achieving the goals according to the designed scenario.
FundingWe have not received funding for the present study.
Conflict of interestThe authors of this article declare no conflict of interest.
To Dr. Jorge Valdez, Dr. Silvia Olivares, Dr. Manuel Pérez and Dr. Ismael Piedra for their leadership in the development of innovative activities at Tec de Monterey School of Medicine, which favor learning in our students and for their support in applying innovative techniques for medical teaching.
To Dr. Elena Ríos and Dr. Isabel García for their support and encouragement in the use of simulation in theoretical courses. To Ing. Joel Martínez for his technical support in using the simulators with students.