This paper considers the development, delivery and implications of interprofessional education (IPE) using a 4-dimensional curriculum development framework. This framework involves: considering curricula for the education of the workforce of the twenty-first century and the rationale for IPE; defining learning outcomes taking into account national and professional accreditation standards; learning activities and assessment; and institutional support.
En este artículo se aborda el desarrollo, la prestación y las implicaciones de la educación interprofesional (EIP) utilizando un marco de desarrollo curricular cuatridimensional. Este marco incluye: la consideración de los planes de estudios para la educación de la plantilla del siglo xxi y el fundamento de la EIP; la definición de los resultados de aprendizaje teniendo en cuenta las normas de acreditación nacionales y profesionales; las actividades de aprendizaje y evaluación, y el apoyo institucional.
Interprofessional education (IPE) is not a recent phenomenon. Early initiatives began in the 1940s in the USA, Canada in the 1960s, Sweden in the 1970s and the UK in the 1980s,1 plus Australia in the 1970s.2 Nor is IPE confined to these countries in the developed western world. In a series of books on leadership for IPE that I am co-editing there are chapters from Kenya, Indonesia and the Philippines as well as India and Japan. As defined by the Centre for the Advancement of Interprofessional Education (CAIPE), IPE has the aim of improving patient care through an interactive learning process: ‘IPE occurs when two or more professions learn with, from and about each other to improve collaboration and the quality of care’ (CAIPE, 2002).3 Its outcomes include teamwork and collaborative practice. The rationale for IPECP (interprofessional education for collaborative practice) varies from country to country. I have discussed these in a review of IPE4 and referred to the Lancet Commission's shared vision and strategy for the education of health professionals.5 The commission highlighted the problem of professional silos, in which health professions are educated and practise separately from each other. Collaborative practice and an understanding of the roles and responsibilities of each health profession are essential for health services to cope with the ageing population and increasing incidence of chronic and complex conditions.
The World Health Organization has long been a supporter of IPECP. Its Framework for Action6 came 22 years after the important document Learning together to work together for health.7 The WHO is driven partly by the recognition that there is a worsening shortage of health care workers globally and that how such workers are educated must be discussed and reframed. This is outlined in the 2013 publication Transforming and scaling up health professionals’ education and training.8 These guidelines are based on the best available evidence in relation to education and make recommendations for changes in policy in areas such as faculty development and pedagogical methods as well as IPE. In relation to IPE the document states that ‘Health professionals’ education and training institutions should consider implementing IPE in both undergraduate and postgraduate programmes’ while recognizing that ‘the quality of the evidence supporting this recommendation is low, and the strength of the recommendation is conditional’ (p.14).
There is certainly a need for more in-depth evaluation9 and research relating to the effectiveness of IPECP. Existing systematic reviews show mixed results and mainly positive outcomes in post-qualification training rather than at the undergraduate level. The Institute of Medicine is currently developing guidelines for research in this area. Also in the USA the National Center for Interprofessional Practice and Education in Minneapolis is conducting longer-term projects across several states. The National Center is funded for five years and is evaluating different models of IPECP to see how they may impact on the triple aim, whose three dimensions are:
- •
Improving the patient experience of care (including quality and satisfaction).
- •
Improving the health of populations.
- •
Reducing the per capita cost of health care.10
In this paper I outline some important factors to consider when developing IPE within a medical programme in partnership with other health professional schools or department, drawing on my own experience and that of colleagues. The structure of the content is based on the 4-dimensional curriculum development framework of Lee et al.,11 which has the following dimensions:
- 1.
Identifying future health care practice needs.
- 2.
Defining and understanding capabilities.
- 3.
Teaching, learning and assessment.
- 4.
Supporting institutional delivery.
It is always difficult to argue the case for adding new learning requirements to medical school curricula. The introduction of IPE into curricula has been difficult in many places due to over full timetables and the logistical problems relating to large numbers of students having to undertake the same learning activities. However, many accreditation bodies have included interprofessional learning outcomes within their standards, prompting an increasing number of medical curriculum committees to look at introducing or developing IPE further in their institutions.
Dimension 1 focuses on the need to develop new or refresh existing curricula to meet the needs of 21st century healthcare. The medical graduates of today will be practising well into the second half of the century and need to be equipped to meet the changing demands and needs of the health service in which they will work and the patients whom they will serve, as well as to understand their global responsibilities as world citizens. IPE development requires a champion to argue eloquently for the need for collaboration, who is interprofessional in outlook, who is able to bring together the various health professions to agree on a common core curriculum and who is up-to-date with the field. Such a champion cannot of course work alone. Each health professional school needs its own champion to join with the others to drive educational change and to plan for longevity. There are so many examples of champions setting up interprofessional activities who then move to another institution (what I have called a ‘championectomy’) after which the interprofessional initiatives wither and disappear. Of course, for success, there must be buy-in from senior leadership within the school and adequate resources for implementation.
Competencies for interprofessional education for collaborative practiceDimension 2 uses the term capabilities but to resonate with most medical curricula I will use the terms learning outcomes and competencies. It is important early on to define the common learning outcomes for all the students who will be involved in IPE. Given the interactive focus of the definition of IPE, the generic learning outcomes for collaborative practice that should be met by all professions require the added value of an interprofessional learning process.12
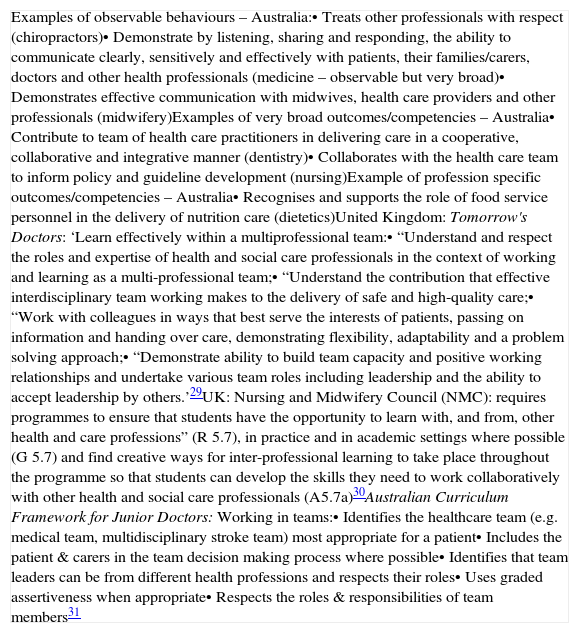
Setting learning outcomes should be based to begin with on the national accreditation standards of each health profession that will be involved with the IPE. It is important that each health profession sees the relevance of this potentially disruptive innovation and can answer the question: ‘what's in it for me?’ There is, however, considerable variation in how accreditation standards are worded as each accreditation program determines its own language. For instance, an analysis of the standards for the ten professions whose national boards are under the jurisdiction of the Australian Health Practitioner Regulation Authority (AHPRA) and which include ‘interprofessional’ related outcomes, revealed that many are very broad, some are very specific to an individual profession, some are general and only some relate to behaviours that may be observed and potentially assessed. Lurie has criticised this type of very broad competency noting that many are abstract and socially constructed concepts, which are difficult to translate into observable and therefore assessable behaviours.13 The accreditation bodies want to know that a health professional graduate is fit to practise as an entry level, which may be translated as ‘competent’. Examples of relevant accreditation standards for individual professions from Australia and the UK are shown in table 1.
Examples from accreditation standards for individual professions from Australia and the United Kingdom.
| Examples of observable behaviours – Australia:• Treats other professionals with respect (chiropractors)• Demonstrate by listening, sharing and responding, the ability to communicate clearly, sensitively and effectively with patients, their families/carers, doctors and other health professionals (medicine – observable but very broad)• Demonstrates effective communication with midwives, health care providers and other professionals (midwifery)Examples of very broad outcomes/competencies – Australia• Contribute to team of health care practitioners in delivering care in a cooperative, collaborative and integrative manner (dentistry)• Collaborates with the health care team to inform policy and guideline development (nursing)Example of profession specific outcomes/competencies – Australia• Recognises and supports the role of food service personnel in the delivery of nutrition care (dietetics)United Kingdom: Tomorrow's Doctors: ‘Learn effectively within a multiprofessional team:• “Understand and respect the roles and expertise of health and social care professionals in the context of working and learning as a multi-professional team;• “Understand the contribution that effective interdisciplinary team working makes to the delivery of safe and high-quality care;• “Work with colleagues in ways that best serve the interests of patients, passing on information and handing over care, demonstrating flexibility, adaptability and a problem solving approach;• “Demonstrate ability to build team capacity and positive working relationships and undertake various team roles including leadership and the ability to accept leadership by others.’29UK: Nursing and Midwifery Council (NMC): requires programmes to ensure that students have the opportunity to learn with, and from, other health and care professions” (R 5.7), in practice and in academic settings where possible (G 5.7) and find creative ways for inter-professional learning to take place throughout the programme so that students can develop the skills they need to work collaboratively with other health and social care professionals (A5.7a)30Australian Curriculum Framework for Junior Doctors: Working in teams:• Identifies the healthcare team (e.g. medical team, multidisciplinary stroke team) most appropriate for a patient• Includes the patient & carers in the team decision making process where possible• Identifies that team leaders can be from different health professions and respects their roles• Uses graded assertiveness when appropriate• Respects the roles & responsibilities of team members31 |
As well as profession-specific outcomes, there are several interprofessional competency frameworks that can be used to reach consensus on setting learning outcomes.14 There are similarities across each framework, and these mirror the types of outcomes for published IPE with the common themes of:
- •
Teamwork
- •
Roles and responsibilities
- •
Communication
- •
Learning/reflection
- •
The patient (client)
- •
Ethics and attitudes12
IPE competency statements ‘identify specific knowledge, skills, attitudes, values and judgments that are dynamic, developmental and evolutionary’.15 For example the Interprofessional Education Collaborative of the United States has defined interprofessional competencies within four domains, and within each domain there are several competencies:
- 1.
Values/ethics
- 2.
Roles and responsibilities
- 3.
Interprofessional communication
- 4.
Teamwork16
The next step and dimension 3 is the development of teaching and learning activities, and subsequent assessment. The learning outcomes must align with the proposed learning activities17 for students and faculty to make sense of why they are working with other health professional students. While ‘learning with’, or common learning, may be appropriate in year 1, thought must be given to the added value of the interprofessional interactive process to facilitate ‘learning from and about’ or shared learning.
The barriers to interprofessional learning activities are well described in the literature and relate in part to the lack of coordination of timetables across multiple schools and curricula. There may be 1000 plus students to accommodate in small groups, in community and hospital settings, online or in person. At least one dedicated full-time interprofessional administrator is required to keep track of students and facilitators. The interprofessional facilitators themselves need training and support.18
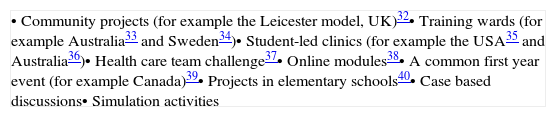
Examples of learning activities are shown in table 2. What is feasible for an institution depends on numbers, clinical placement opportunities, the local and national health services and the timing and length of any activity. As with all clinical education it is impossible that every student should have exactly the same experiences. The important consideration is that every student should be given equal opportunity to meet the defined learning outcomes and develop the required competencies.
Examples of learning activities for interprofessional learning outcomes.
| • Community projects (for example the Leicester model, UK)32• Training wards (for example Australia33 and Sweden34)• Student-led clinics (for example the USA35 and Australia36)• Health care team challenge37• Online modules38• A common first year event (for example Canada)39• Projects in elementary schools40• Case based discussions• Simulation activities |
Ideally students should become members of teams and be exposed to the complex tasks and boundary challenges of decision-making and service delivery in such teams and wider collaborations in order for interprofessional learning to occur. We know that situated and experiential learning is enhanced through continuity of location and supervision.19 However it is not clear how long a specific clinical attachment needs to be in order for students to feel part of a team or community of practice.20 As students move from one community of practice21 to the next, they need time to build trust with their colleagues, supervisors and patients/clients. Building trust is facilitated when students are able to have longitudinal clinical placements.19 However health professional clinical rotations are frequently of unequal lengths that limit the ability of students to experience teamwork in vivo.
AssessmentWithout some form of assessment we cannot know whether students have learnt and have achieved the defined outcomes. Moreover, medical students are known to base their evaluation of a subject's importance on whether it is assessed (‘assessment drives learning’). Assessment therefore has educational impact,22 which can be enhanced by the provision of feedback to learners on their strengths and areas for improvement. While assessment has been referred to as either summative or formative, these two properties should not be mutually exclusive. Though summative assessment compares a learner's achievement through marks or grades with a previously set standard in order to make decisions about progression, it is also an opportunity for further learning. Assessment is a process that should provides information to both learners and educators about the achievements and progress of the learner. Assessment of skills-based activities and complex tasks such as teamwork requires a formative component with observation followed by constructive and timely feedback. When done well it is thus time and resource intensive.
As noted above students infrequently work in defined interprofessional teams for any length of time, and therefore observation of their teamwork and collaborative practice skills is difficult. A way round this is to form a team specifically for the purpose of assessment, for example for a T-OSCE (teamwork objective structured clinical observation)23 in a simulated setting. While this type of ‘teamwork’ may mimic such activities as the response to a cardiac arrest, it does not indicate how students perform in more established teams. A ‘team’ of students brought together to be assessed for their collaborative skills is unlikely to function that well.24 Dunworth has shown that educational cultures across the professions vary and are barriers to the development of acceptable and feasible assessments for interprofessional learning outcomes and competencies.25
In the workplace students are often reluctant to solicit feedback; they may not be sure who to seek out in the busy environment and may consider that only feedback from someone of their own profession is relevant and acceptable for work-based assessment purposes. Current educational experts recommend that feedback should no longer be viewed as a passive activity on the part of the learner: ‘the information provided to students is used to influence their subsequent task performance’.26 Students are encouraged to be active and indeed seek out feedback rather than wait for it to happen.
There are a number of instruments for the assessment of teamwork using behavioural markers for the observation of healthcare teams; many are quite complex and assume that teams have been working together for sometime. Multisource feedback (MSF), also known as 360 degree appraisal, promotes learning and leads to improvement depending on the quality and timing of the feedback including negative feedback.27 However MSF is collected over time from different stakeholders and is not specific to teamwork tasks or activities. MSF forms are completed by a variety of appraisers, who may include self, peer, own profession clinicians, other health professionals and, sometimes, patients, service users and carers. MSF and other WBA best practice suggests that they are kept simple with few items, but there is a lack of consensus as to how many assessors (or appraisers) are needed.28 Self and peer assessment are being increasingly used as a means of assessing group and teamwork in university settings.
One solution to the difficulty of assessing large number of students at the same time is to introduce an interprofessional portfolio. Students provide evidence of how they have met the defined interprofessional learning outcomes for their program and professional accreditation standards. A range of learning activities are provided by the institution, such as those listed in table 2, and students choose which activities they will undertake or are allocated to activities depending on their attachments and other commitments. The portfolios are scrutinised by a mentor or supervisor, or are discussed in student supervised groups. If necessary and feasible, a certain proportion of portfolios are quality assured to motivate students to complete them satisfactorily. In future an interprofessional portfolio may become a requirement of a health service employer to ensure that qualifying health professional are fit for purpose in a team-based delivery system.
Conclusion and implicationsAs interprofessional learning outcomes and/or competencies are increasingly being required by health professional accreditation standards, universities and their medical schools need to consider how to implement IPE within their curricula. Dimension 4 of the 4-dimensional curriculum development framework emphasises the need for institutional support for IPE to succeed and be sustainable. Interprofessional faculty discussions are necessary to define outcomes in common and develop a suite of interprofessional activities to help students achieve the required learning. Assessment remains a difficult issue given the large number of students across schools and faculties. New ideas in assessment may be required and evaluation continues to be important to add to the evidence for the impact of IPE for future practice.