To analyse the effectiveness of Paediatric Basic Life Support (PBLS) and Paediatric Immediate Life Support (PILS) courses to train medical students in paediatric cardiopulmonary resuscitation (CPR).
MethodsEighteen courses (13 in PBLS and 5 in PILS) were delivered to 1214 medical students. Two theory tests and one practical test were performed. Students filled in an anonymous questionnaire after each course.
ResultsThe mean scores (out of 20) in the theory tests of the PBLS course were 11.4 before the course, and 19.2 upon completion (P<0.0001). Infant BLS skills were achieved by 98.4% of students, and children BLS skills by 97% of them. The mean scores (out of 30) in the PILS courses were 17.3 before the course, and 29.1 at the end of the course (P<0.0001). PBLS skills were achieved by 99% of students and PILS skills by 98.3% of them. The scores (out of 5) in the anonymous questionnaire were: theory classes, 4.5; teaching methods, 4.5; practice sessions, 4.7; instructor teaching skills, 4.8; and coordination of theory and practice and between instructors, 4.7. There were no significant differences between basic and intermediate CPR courses.
ConclusionsPBLS and PILS courses are useful methods for delivering theory and practice training to medical students, and should be mandatory in the paediatric curriculum of medical studies.
Analizar la utilidad de cursos de reanimación cardiopulmonar básica (RCPB) e intermedia (RCPI) para la formación de los estudiantes del grado de medicina.
MétodosSe impartieron 18 cursos (13 de RCPB y 5 de RCPI) a 1.214 estudiantes de medicina. Se realizaron 2 exámenes teóricos uno inicial y otro final, y una evaluación práctica. Después del curso los estudiantes realizaron una encuesta anónima.
ResultadosEn el curso de RCPB la puntuación en el examen inicial fue de 11,4 sobre 20 y 19,2 en el examen final (p<0,0001). Un 98,4% de los estudiantes del curso de RCPB adquirieron suficiente práctica en la RCP del lactante y 97 en la RCP del niño. En el curso de RCPI la puntuación en el examen inicial fue de 17,3 sobre 30 y 29,1 en el examen final (p<0,0001). Un 99% de los estudiantes del curso de RCPB adquirieron suficiente práctica en la RCP básica y un 98,3% en la RCP intermedia. Las valoraciones en la encuesta anónima (sobre 5) fueron: clases teóricas 4,5; métodos de enseñanza 4,5; prácticas 4,7; capacidad docente de los profesores 4,8, y coordinación teórico-práctica y entre instructores 4,7. No existieron diferencias entre los cursos de RCP básica e intermedia.
ConclusionesLos cursos de RCP pediátrica básica e intermedia son métodos útiles para la formación teórica y práctica de los estudiantes de medicina y deberían incluirse como obligatorios en el currículum del grado de medicina.
Cardiac arrest in children carries a high mortality.1,2 Morbidity and mortality can only be reduced by correct cardiopulmonary resuscitation (CPR) initiated in the first minutes after the arrest.1,2 This makes it necessary not only for healthcare professionals but also for the general population to learn CPR. However, the ability to perform correct CPR requires both theoretical knowledge and, very importantly, practical training and proficiency.
CPR training for medical students is essential to ensure that all doctors are able to perform it correctly. However, CPR is still not a mandatory subject in medical faculties in many countries.3–7
Over the last years, some medical faculties have included CPR training in their curricula, using various theory and practice programs and methods.8–17 The majority of these programs have focused on training in basic adult CPR, as cardiac arrest is much more common in the adult than in the child.8–13
However, characteristics of cardiac arrest in children differ from those in adults, including the causes and mechanisms of arrest, preventive measures, resuscitation manoeuvres and devices, all of which require specific training. In addition, differences also exist between different paediatric age groups. Doctors should therefore receive specific training in paediatric CPR.
Few medical faculties provide training in paediatric CPR as part of their curriculum.14–17 The majority of universities still do not have a structured training program and, in those in which it exists, the focus is mainly on basic CPR. As a result, training in paediatric CPR among medical students and recently qualified doctors is insufficient.
Our hypothesis was that it is possible to organise training in basic and immediate paediatric CPR within the paediatric curriculum of medical studies and that students can achieve adequate theoretical knowledge and practical abilities in basic paediatric CPR as well as in immediate paediatric CPR.
The objective of the present study was to analyse the efficacy of training courses in basic and immediate paediatric CPR for medical students and to compare the results between the two types of courses.
MethodsWe performed a retrospective analysis of a prospective single-centre study that analysed the paediatric CPR courses undertaken by fifth-year medical students. These courses were organised by the Paediatric Intensive Care Unit of Gregorio Marañón General University Hospital as part of the Paediatrics Department of the Complutense University in Madrid, which is the largest University in Spain. Each year, between 300 and 450 students enter the fifth year (out of six) of medical training, when they receive their education in Paediatrics. This includes a two-month clinical rotation in the Department of Paediatrics. They have to choose between three different hospitals for their clinical rotations. Between 110 and 140 fifth-year students undertake their paediatric rotation in the Gregorio Marañón University Hospital.
Between 1998 and 2015, 18 theory-practice CPR courses were delivered (13 in basic paediatric CPR and 5 in immediate paediatric CPR) to fifth-year students from the Gregorio Marañón University Hospital. The courses were accredited by and followed the teaching methodology of the Spanish Paediatric and Neonatal Cardiopulmonary Resuscitation Group (SPNCRG), the Spanish Cardiopulmonary Resuscitation Council and the European Resuscitation Council.
The same two directors coordinated all courses. All teachers were accredited Paediatric Resuscitation Instructors by the SPNCRG (4 were associate Professors in Paediatrics from the School of Medicine of the Complutense University of Madrid and the remainder were collaborating Paediatric Resuscitation Instructors).
In the initial years, student participation in the CPR courses was voluntary and the courses were given outside normal teaching hours. In later years, the CPR courses were mandatory and were included in the paediatrics curriculum.
The study was approved by the Gregorio Marañón University Hospital ethics committee. At the beginning of each course, written informed consent for participation in the study was obtained from participants.
The duration of the paediatric basic life support (PBLS) courses for each student was 6h, divided in two days. The paediatric immediate life support (PILS) courses had a duration of 12h for each student over three days. Time allocation was identical in the two courses: theory (35%), practice (50%), and evaluation (15%).
Theory lessons in the PBLS course were given in two sessions: the concepts of cardiac arrest in childhood, methods of prevention, and basic paediatric CPR.
Theory lessons in the PILS course were given in five sessions: concepts of cardiac arrest in children and methods of prevention; basic paediatric CPR; airway, vascular access and drugs; arrhythmias; and integrated immediate CPR.
One or two CPR instructors gave each practice session. In both courses, students were divided into groups of five to seven individuals for the practice sessions to allow all students to practice each manoeuver and clinical scenarios. Each day of practice training included four groups of students, so it took 4–6 days to deliver all practice sessions in each course. Methodology was similar in all practice sessions. The instructor performed the technique first, acting as a model, and then presented a series of clinical cases so that each student could practise each one of the CPR techniques and the full CPR sequence on clinical scenarios. After the practice session, students were asked to self-evaluate their performance, which was then discussed in a constructive manner by their colleagues and, finally, by the instructor, who drew attention to the most important points for improvement.
The basic paediatric CPR included two practical sessions, one on basic infant CPR with the ResusciBaby® manikin and the other one on CPR in the child, using the ResusciJunior® manikin (Laerdal).
The PILS course included three practice sessions: basic paediatric CPR with the semiautomatic defibrillator for children; immediate CPR techniques (cervical stabilisation, airway and ventilation, intraosseous vascular access, and drug administration) and integrated CPR practice.
The advanced paediatric CPR manikin (MegacodeJunior®, Laerdal) was used for the practice sessions of immediate CPR; the paediatric intraosseous leg trainer and chicken bones were used to practice intraosseous access. The following complementary material was also used: infant and paediatric bag-mask, oropharyngeal (Guedel) airway, aspiration cannula, intraosseous catheter and syringes for medication. During integrated immediate paediatric CPR, students worked in teams to treat simulated cases of cardiac arrest in children in order to learn to perform and coordinate the techniques and to direct, coordinate, and distribute the workload.
Students had to take two theory tests, one at the beginning and one at the end of each course, in order to assess student proficiency. Two question formats were used, according to the recommendations of the Spanish Paediatric and Neonatal CPR Group. First, multiple-choice questions with five possible options, which evaluated the main practical aspects of paediatric CPR based on clinical situations. Then, students were asked to put in the correct order the sequential steps of basic or immediate paediatric CPR.
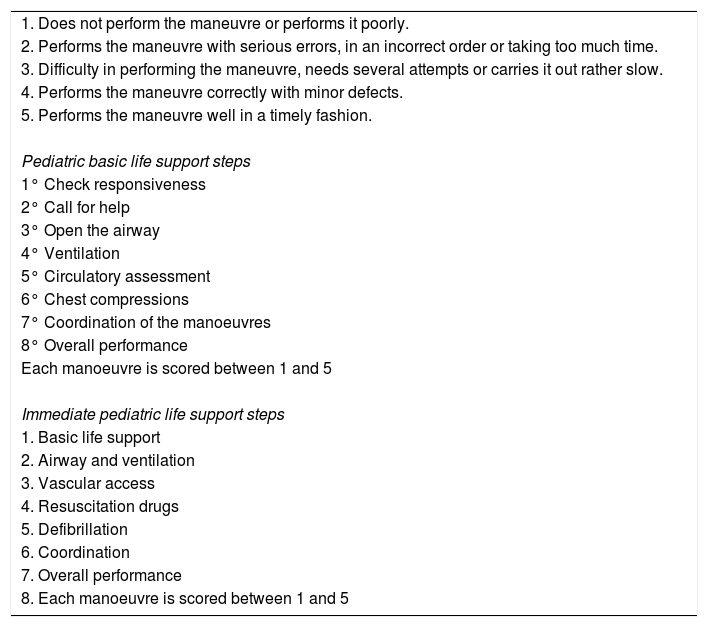
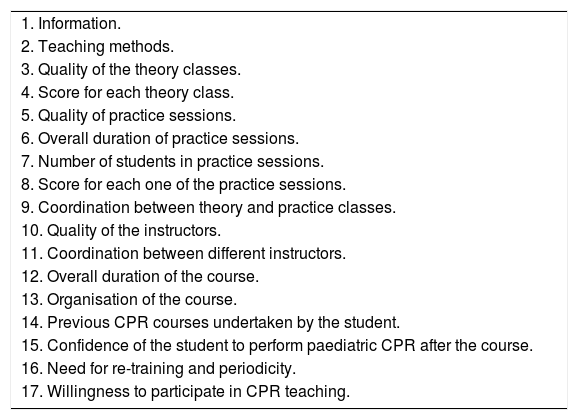
Theory tests in the course of basic CPR had 20 questions (Annex 1); students were considered to have acquired a sufficient level of knowledge if they answered correctly 80% of questions. Practice tests of basic and immediate CPR included student performance in different clinical cases. A score between 1 and 5 points was assigned to each manoeuver of basic CPR (evaluation of responsiveness, call for help, opening the airway, ventilation, circulatory assessment and chest compressions, coordination and overall performance) and immediate CPR (basic CPR, airway and ventilation, vascular access, drugs, semiautomatic defibrillation, coordination, and overall performance). Table 1 shows practice skills and evaluation criteria. Evaluation criteria were established by a consensus of experts in the Spanish Paediatric and Neonatal Group.14 All instructors were trained in these evaluation criteria to ensure the best concordance. Students were considered to have achieved sufficient practice skills when they performed all the manoeuvres in a coordinated manner and achieved an overall score of at least 3 points. At the end of each course, students filled in an anonymous evaluation of the course, analysing the quality of theory and practice and whether or not periodic training was necessary. This questionnaire is summarised in Table 2.
Evaluating criteria for the practice exam.
| 1. Does not perform the maneuvre or performs it poorly. |
| 2. Performs the maneuvre with serious errors, in an incorrect order or taking too much time. |
| 3. Difficulty in performing the maneuvre, needs several attempts or carries it out rather slow. |
| 4. Performs the maneuvre correctly with minor defects. |
| 5. Performs the maneuvre well in a timely fashion. |
| Pediatric basic life support steps |
| 1° Check responsiveness |
| 2° Call for help |
| 3° Open the airway |
| 4° Ventilation |
| 5° Circulatory assessment |
| 6° Chest compressions |
| 7° Coordination of the manoeuvres |
| 8° Overall performance |
| Each manoeuvre is scored between 1 and 5 |
| Immediate pediatric life support steps |
| 1. Basic life support |
| 2. Airway and ventilation |
| 3. Vascular access |
| 4. Resuscitation drugs |
| 5. Defibrillation |
| 6. Coordination |
| 7. Overall performance |
| 8. Each manoeuvre is scored between 1 and 5 |
Areas covered in the course assessment questionnaire.
| 1. Information. |
| 2. Teaching methods. |
| 3. Quality of the theory classes. |
| 4. Score for each theory class. |
| 5. Quality of practice sessions. |
| 6. Overall duration of practice sessions. |
| 7. Number of students in practice sessions. |
| 8. Score for each one of the practice sessions. |
| 9. Coordination between theory and practice classes. |
| 10. Quality of the instructors. |
| 11. Coordination between different instructors. |
| 12. Overall duration of the course. |
| 13. Organisation of the course. |
| 14. Previous CPR courses undertaken by the student. |
| 15. Confidence of the student to perform paediatric CPR after the course. |
| 16. Need for re-training and periodicity. |
| 17. Willingness to participate in CPR teaching. |
All data were prospectively recorded. SPSS version 21.0 software package was used for statistical analysis of the results. A paired samples comparison test was used to compare scores between the initial and final theory test. A multiple measures ANOVA test was used to compare results between years. The Student t-test for independent samples was used to compare the scores of basic and immediate CPR courses.
ResultsIn total, 1214 students participated in the 18 paediatric CPR courses: 738 (60.8%) in the PBLS course between 1998 and 2010, and 476 (39.2%) in the PILS course between 2011 and 2015.
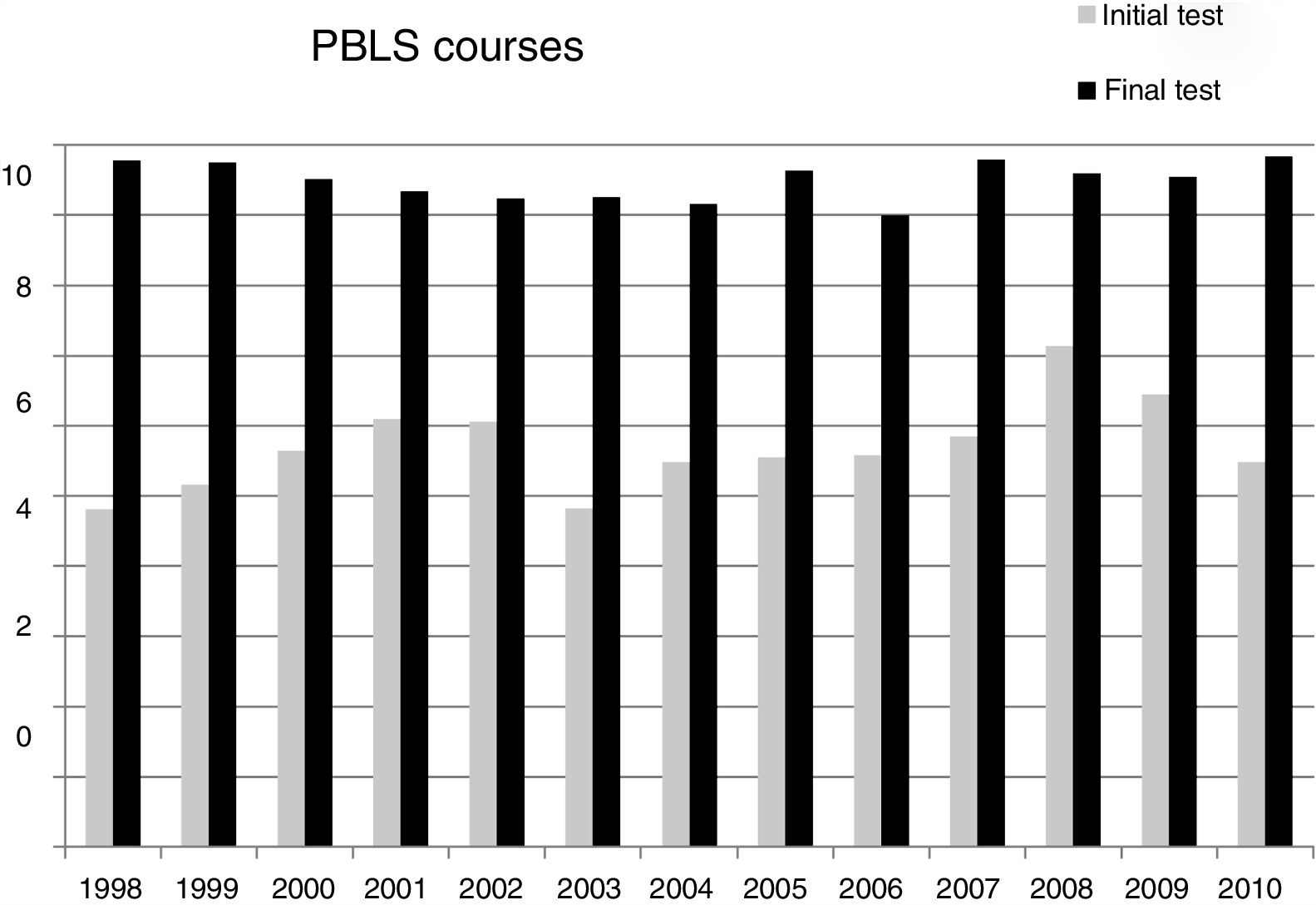
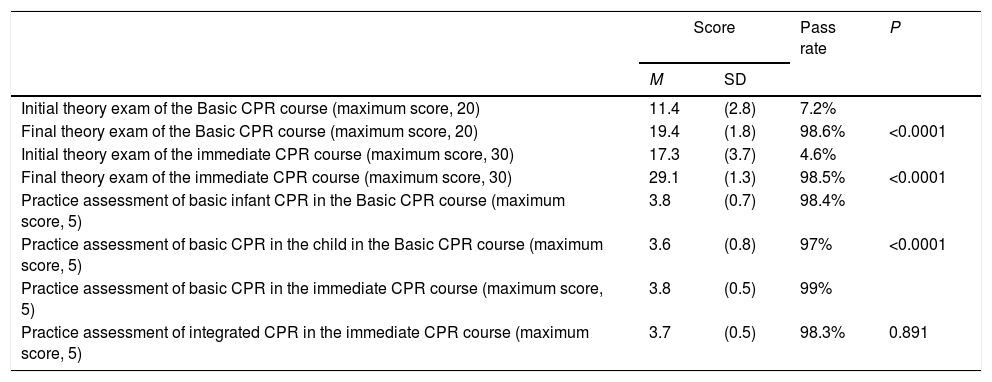
Basic paediatric CPR coursesIn the initial theory test, the mean score was 11.4 out of a maximum of 20, and 19.2 in the final theory test (P<0.0001), showing a mean increase of 39%. The percentage of students who attained the pass mark (>80% of answers) increased from 7.2% in the initial exam to 98.6% in the final exam.
In the practice test, the mean score was 3.8 for basic infant CPR and 3.6 for basic paediatric CPR, out of a maximum of 5 points. The pass rate for the practical exam was 98.4% for basic infant CPR and 97% for paediatric CPR (Table 3).
Results of the and theory and practice tests of the basic and immediate pediatric resuscitation courses.
| Score | Pass rate | P | ||
|---|---|---|---|---|
| M | SD | |||
| Initial theory exam of the Basic CPR course (maximum score, 20) | 11.4 | (2.8) | 7.2% | |
| Final theory exam of the Basic CPR course (maximum score, 20) | 19.4 | (1.8) | 98.6% | <0.0001 |
| Initial theory exam of the immediate CPR course (maximum score, 30) | 17.3 | (3.7) | 4.6% | |
| Final theory exam of the immediate CPR course (maximum score, 30) | 29.1 | (1.3) | 98.5% | <0.0001 |
| Practice assessment of basic infant CPR in the Basic CPR course (maximum score, 5) | 3.8 | (0.7) | 98.4% | |
| Practice assessment of basic CPR in the child in the Basic CPR course (maximum score, 5) | 3.6 | (0.8) | 97% | <0.0001 |
| Practice assessment of basic CPR in the immediate CPR course (maximum score, 5) | 3.8 | (0.5) | 99% | |
| Practice assessment of integrated CPR in the immediate CPR course (maximum score, 5) | 3.7 | (0.5) | 98.3% | 0.891 |
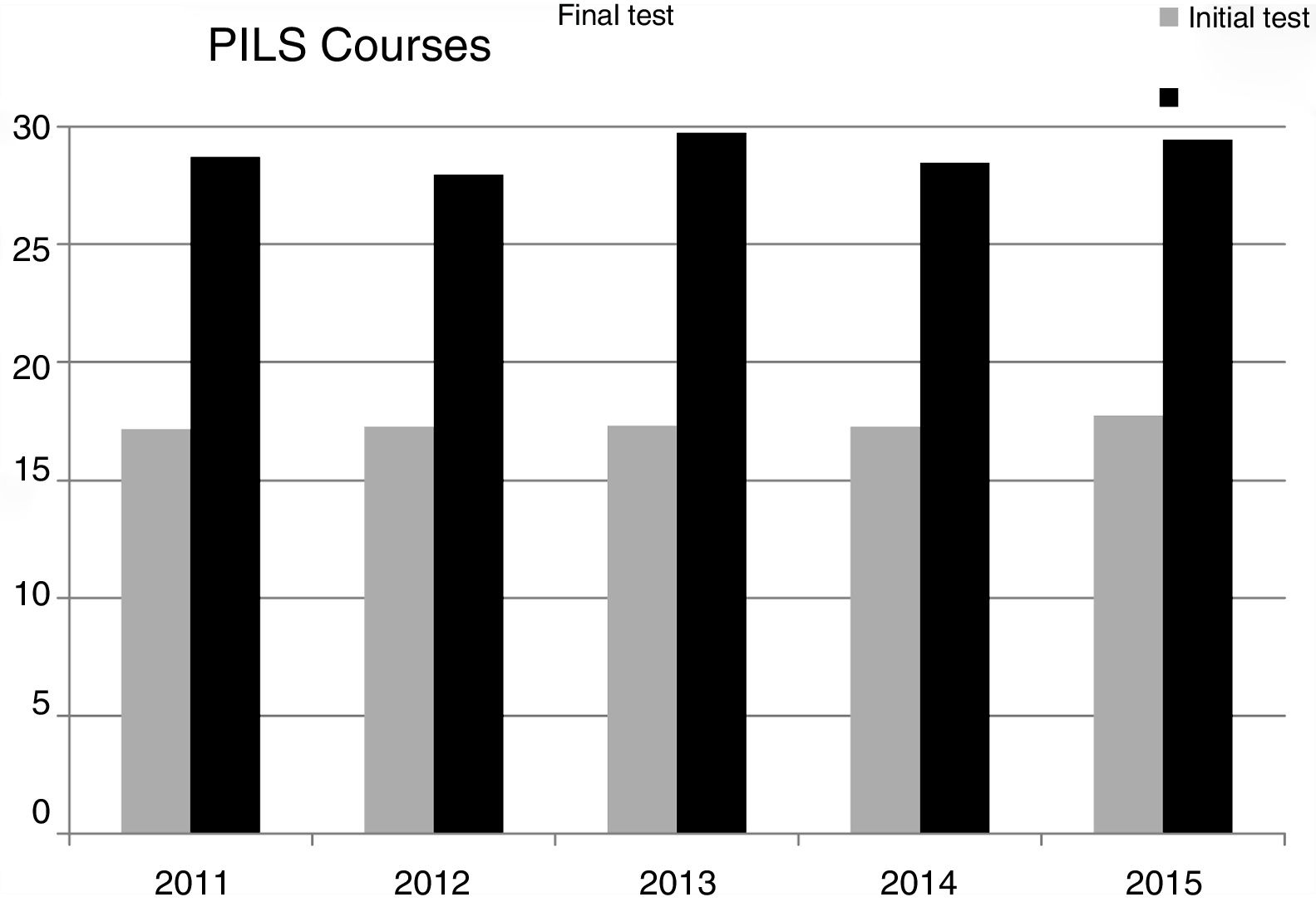
In the initial theoretical exam, the mean score was 17.3 out of a maximum score of 30, and in the final theoretical exam, the mean score was 29.1 (P<0.0001), which is an increase of 38.7%. The pass rate increased from 4.6% in the initial exam to 98.6% in the final exam.
In the practice test, the mean score in basic CPR was 3.8 and in immediate CPR was 3.7. The pass rate for the practice test was 99% for basic CPR and 98.3% for immediate CPR (Table 3).
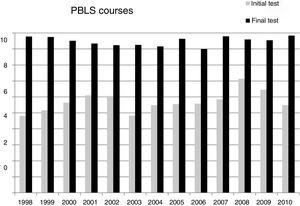
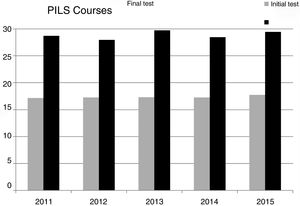
Comparison between basic and immediate CPR coursesIn order to compare the theory test of the two courses, the scores were normalised to a maximum of 10 points. The initial and final scores of the PBLS courses (5.7 and 9.6, respectively) were similar to those of the PILS courses (5.8 and 9.7, respectively). Likewise, no significant differences were observed in the percentage of passing students between the two courses. Nor were there any significant differences when comparing the results of the series of 13 basic CPR courses or the series of five immediate CPR courses (Figs. 1 and 2).
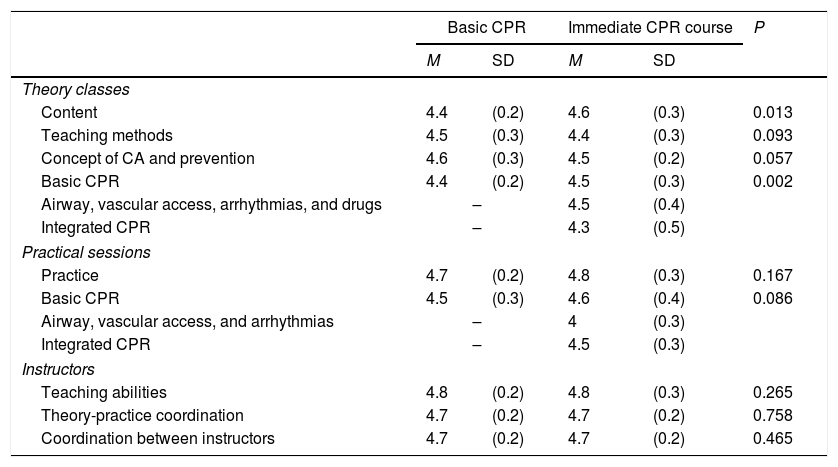
All 1214 students (738 for basic paediatric CPR and 476 for immediate paediatric CPR) filled in the course evaluation survey. Results are summarised in Table 4. The majority of students considered that the theoretical information received was adequate (Table 4). The theory contents of the PILS courses received a slightly higher score than the PBLS course. The majority of students considered the practice sessions for both courses adequate, and there were no significant differences between the two courses. Nor were there any differences in the evaluation of the teaching abilities of the staff, the theory-practice coordination, and the coordination between instructors (Table 4).
Feedback from the students.
| Basic CPR | Immediate CPR course | P | |||
|---|---|---|---|---|---|
| M | SD | M | SD | ||
| Theory classes | |||||
| Content | 4.4 | (0.2) | 4.6 | (0.3) | 0.013 |
| Teaching methods | 4.5 | (0.3) | 4.4 | (0.3) | 0.093 |
| Concept of CA and prevention | 4.6 | (0.3) | 4.5 | (0.2) | 0.057 |
| Basic CPR | 4.4 | (0.2) | 4.5 | (0.3) | 0.002 |
| Airway, vascular access, arrhythmias, and drugs | – | 4.5 | (0.4) | ||
| Integrated CPR | – | 4.3 | (0.5) | ||
| Practical sessions | |||||
| Practice | 4.7 | (0.2) | 4.8 | (0.3) | 0.167 |
| Basic CPR | 4.5 | (0.3) | 4.6 | (0.4) | 0.086 |
| Airway, vascular access, and arrhythmias | – | 4 | (0.3) | ||
| Integrated CPR | – | 4.5 | (0.3) | ||
| Instructors | |||||
| Teaching abilities | 4.8 | (0.2) | 4.8 | (0.3) | 0.265 |
| Theory-practice coordination | 4.7 | (0.2) | 4.7 | (0.2) | 0.758 |
| Coordination between instructors | 4.7 | (0.2) | 4.7 | (0.2) | 0.465 |
More than 20% of the students in the PBLS courses considered that the duration of the course and the practice sessions was too short, and requested a more advanced course. However, only 8% of the students in the PILS courses considered that the duration was too short.
Student self-evaluationThe majority (58.8%) of students had previously received some training in CPR, but always in basic adult CPR. After performing the course, 90% of students felt ready to perform paediatric CPR (84.5% of the students in the PBLS courses and 97.3% of students in the PILS courses) (P=0.038).
Almost all (99.3%) students considered it necessary to perform periodic retraining (50.4% every year and 26.3% every two years).
DiscussionAt present, the majority of faculties of medicine do not count with a structured adult or paediatric CPR training program. Very few faculties include specific paediatric CPR training in their curriculum, and those that do have them are mostly limited to basic CPR.15–18 Our study shows that it is possible to organise basic and immediate paediatric CPR training for medical students in a university with a large number of students and to integrate this training into the paediatric rotation of the curriculum. Our model has served as the basis for setting up paediatric CPR training in the other hospitals linked to our university and could be extended to other universities across the world.
In our study, the initial theory test showed that medical students had a poor knowledge of paediatric CPR prior to the course. Only 7.2% of students in the basic CPR courses and 4.6% of those in the immediate CPR courses had sufficient theoretical knowledge, even though 60% of students had previously received some form of training in CPR. These findings demonstrate that, in the absence of a specific course in paediatric CPR, the majority of medical graduates have insufficient knowledge and practical competence in paediatric CPR. This highlights the need to establish structured CPR training for medical students.18
Our study also demonstrates that medical students are able to acquire the theoretical knowledge and practice skills and competence in both basic and immediate CPR. There were no significant differences between the courses, and both basic and immediate CPR courses are appropriate methods for this training.
Some studies have evaluated medical student training in paediatric CPR using courses of different lengths and with different teaching methodologies. Some authors have used self-training with digital media, which allows for better time organisation and repetition of the theory program according to the needs of the student, but this must be associated with supervised on-site sessions to guarantee a sufficient level of learning to perform quality CPR.16,19–21 Other studies have used training methods in which the students act as the teachers of their peers or of residents.22 There is no doubt that this method favours the scope of training, but it can affect the quality of teaching, as the students have less experience in CPR and in the role of instructor.
In our study, paediatricians with a broad experience in CPR (accredited as paediatric CPR instructors) performed the theory and practice training in CPR on-site, thus guaranteeing high-quality training.
However, this system is more time and staff-consuming. Thus, universities with a large number of students need to ensure the availability of sufficient teaching staff in this area.
Practice sessions are a crucial part of all CPR courses as they improve mastery of the individual techniques and, in particular, reinforce the learning of the correct sequence and rhythm of actions. These aspects can only be learned in a safe environment that simulates real-life situations using manikins. The duration of our courses and the time dedicated to the practice sessions were longer than other courses.23 It is very important that the course have a sufficient duration to allow each student to practise each manoeuvre and the combined sequence on clinical scenarios. The results of our studies show that the time dedicated to practice sessions was adequate, as the majority of students acquired the expected skills and most students considered that the time dedicated to hands-on practice was sufficient.
In this study, we have analysed training in paediatric CPR in a large number of medical students over a long period. We believe this is the largest study in this field and the only one to compare training in basic CPR and immediate CPR. The results of both the basic and the immediate CPR courses were homogeneous over time, confirming that the organisation and teaching methodology were appropriate and that course quality was maintained.
The course assessment questionnaire is a key method to identify and analyse possible deficiencies and thus improve course quality. In our study, students gave a very positive evaluation not only of the theory and practice contents but also of the organisation and teaching methodology. A large proportion of the basic CPR students considered that the course was too short and expressed a desire to receive broader training, as they considered that they could acquire additional knowledge and skills according to the needs of their future professional practice.
At the end of the course, the majority of students considered themselves able to perform paediatric CPR. The percentage was higher for the PILS courses, which probably reflects the greater self-confidence achieved by receiving a more complete training.
LimitationsAn important factor in CPR is to analyse whether the knowledge and skills acquired during a course is maintained over time. Our study only analysed the acquisition of theoretical knowledge and skill competence at the end of the course; we did not analyse whether this competence was maintained over time. Some studies show that, among medical students, there is a significant loss of competence in CPR within a year after the training.24
Many instructors participated as teachers through the study and it is not possible to analyse the effect of variability between teachers. However, all teachers were accredited instructors by the SPNCRG. Moreover, evaluation criteria were continuously assessed to guarantee a homogeneous teaching and evaluation methodology, as supported by the fact that no significant differences were found in the results of the student assessment of the course.
ConclusionsWe conclude that basic and immediate paediatric CPR courses are good methods for training medical students in paediatric CPR. Our model could serve as a basis for the design of structured immediate paediatric CPR training courses to be included in university medical curricula.18
FundingNone.
Conflict of interestAll authors declare no conflicts of interest.
Andrés Alcaraz, Ángel Carrillo, Nieves de Lucas, Sarah Fernández, Cristina García, Rafael González, Jorge López, Jesús López-Herce, Oscar Martínez, Ana María Morito, Santiago Mencía, Silvia Pérez, Marta Rupérez, María José Solana, Amelia Sánchez, César Sánchez, María José Santiago, Blanca Toledo, and Javier Urbano.