The management of a difficult airway requires training in cricothyroidotomy (CT). The objectives of this study were: (i) to describe technical changes made to The REAL CRIC Trainer model in order to increase its realism, (ii) to assess the model by experts in comparison to a commercial dry model, (iii) to evaluate its performance in a realistic simulation scenario for training technical and behavioural skills, and (iv) to assess whether the model can help to identify anatomic structures by ultrasound (US).
MethodsAn observational prospective study was conducted in which an assembled modified model was assessed by five experts in CT and comparing it with a commercial dry model. The fidelity of US images obtained in the model was compared to those obtained from volunteers. The usefulness and realism of the model, attached to a high-fidelity simulator's neck in emergent CT clinical scenario, was assessed by the 11 ICU staff taking part.
ResultsUsing a score out of 10, CT performance in our model and in a dry model was rated by the experts as 9 vs. 6, respectively in external appearance, 8.4 vs. 5.8 in tactile fidelity, and 8.6 vs. 4.1 in technical realism. Participants in the simulation gave a mean score of 7.7/10 to the fidelity parameters. Usefulness for training of the model integration into a simulation scenario was rated as 9.6. Ultrasound images were evaluated as high fidelity.
ConclusionsOur modified REAL CRIC Trainer model was rated high by experts in CT and participants in a simulated clinical scenario, and may be useful for a complete emergent CT training closer to the clinical reality than the models currently available.
El manejo de la vía aérea difícil comprende el entrenamiento en la cricotiroidotomía (CT). Los objetivos de este estudio fueron: describir los cambios técnicos realizados en el modelo REAL CRIC Trainer para aumentar el realismo, obtener su valoración por expertos respecto a un modelo seco comercializado, evaluar su rendimiento en un escenario de simulación para el entrenamiento de habilidades técnicas y conductuales de la CT emergente y determinar si el modelo permite identificar estructuras anatómicas mediante ecografía.
MétodosEstudio prospectivo y observacional, el modelo ensamblado fue evaluado por 5 expertos en CT que lo compararon con un modelo seco comercial. Se comparó también su fidelidad ecográfica con la de las imágenes obtenidas en voluntario. La utilidad y el realismo del modelo utilizado en un escenario de simulación clínica para CT emergente fue valorada por 11 participantes, personal de la UCI.
ResultadosLa evaluación por expertos de la CT en el modelo diseñado y en modelo seco comercial, obtuvo puntuaciones de 9 vs. 6 sobre 10, respectivamente en apariencia externa, 8,4 vs. 5,8 en fidelidad táctil y 8,6 vs. 4,1 en realismo de la técnica. Los participantes en la simulación otorgaron una puntuación media de 7,7/10 a los parámetros de fidelidad. La utilidad de integrar el modelo en un escenario de simulación de alta fidelidad fue evaluada en 9,6/10 y las imágenes de ultrasonido fueron consideradas como de alta fidelidad.
ConclusionesEl modelo REAL CRIC Trainer modificado fue muy bien valorado tanto por los expertos como por los participantes en un escenario clínico de simulación, y puede ser útil para un entrenamiento completo en CT emergente más próximo a la realidad clínica que los modelos disponibles.
Nowadays, the airway management continues being a potential source of serious complications. The difficult airway (DA) prediction parameters have a limited value due to great interindividual variability.1 Despite new algorithms and devices,1,2 the cricothyrotomy is still the rescue subglottic access in a “can’t intubate, can’t oxygenate” situation (CICO),3 and therefore, all professionals dealing with the airway should master this technique. However, due to its low frequency and the extremely stressful context, this technique becomes cognitively complex, being necessary training both, psychomotor and behavioural competences.
Clinical simulation allows acquiring and evaluating technical and non-technical skills in a safe learning environment for participants and patients. Recently a low-cost high fidelity phantom called REAL CRIC Trainer (RCT) has been described by Kei et al.4 This model is composed of a 3D printed trachea covered with pork belly which allows air and blood outlet, conferring a high degree of realism, however, there is no information about its application in the training process.
The main objective of this study was to increase the realism of the RCT model, to compare it with a dry commercial model by cricothyrotomy experts and to assess its performance for training technical and behavioural skills in a simulated CICO situation. Another objective was to assess if the model allowed, the identification of anatomical structures by ultrasonography.
MethodsAn observational unicentric study, developed between March 2019 and June 2020. It was submitted to the Ethics & Research Committee of Hospital and exemption was obtained (n° 12/2020). The study adjusted to the ethical standards of the Declaration of Helsinki, written informed consent was not necessary because no patient data has been included in the manuscript.
The STROBE checklist guided the methods and structures of this manuscript (Appendix 1a)
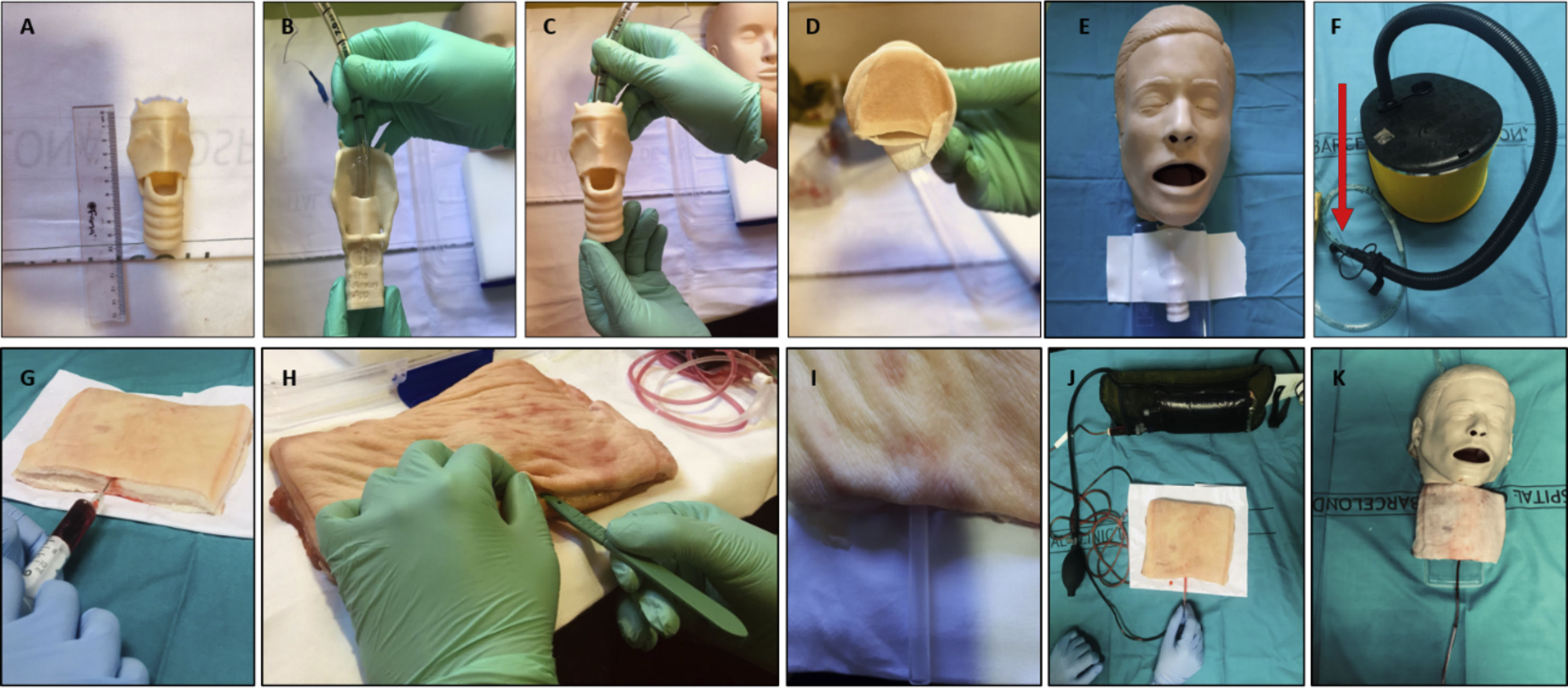
Phantom design process and integration in a realistic simulation scenarioTo increase the realistic sensations of the RCT model we performed some changes in the RCT,4 these were regarding air and blood outlet. A 3D trachea was printed as originally described4 from the following STL file: http://www.airwaycollaboration.org/3d-cric-trainer-1/ (Fig. 1E, Fig. 2), The elements are assembled sequentially as shown in Fig. 1, costs are shown in Appendix 1b, being the total cost 220 Euro.
- -
Air outlet. In the original RCT air input to simulate its leakage when penetrating the cricothyroid membrane is performed from an endotracheal tube (ETT) connected to an Ambu bag. We changed the bag for an air pump operated by the instructor's foot away from the participant. (Fig. 1F)
- -
Blood outlet. In the RCT the blood input is obtained by means of an intravenous infusion set with its distal end tunnelled into the pork belly and its proximal end connected to a 1L bag of saline, stained red with food dye. The instructor must manually tighten the bag at the exact moment in which the participant makes the incision in the skin. The instructor needs to dedicate one hand solely to manage the blood flow (as with the air flow) and the pressure exerted does not overcome the resistance of the tissue. In our modified RCT an artificial blood bag is externally squeezed by putting it in a pressurizer. As a result, the instructor got released and the pressure exerted is greater and constant (Fig. 1J).
- -
Tunnelling of pork belly. In the original RCT tunnelling of pork loin to introduce the intravenous infusion set with stained serum is simply done with a scalpel incision 0.5cm deep, reaching the place where the participant should make the cricothyroid membrane incision. Performing the tunnelling in this way was difficult and in some cases the tissue resistance was higher than the blood pressure, impeding the blood outlet though the incision, we advanced the tunnelling further, beyond the expected place of the incision to diminish tissue resistance and thus allowing blood outlet. The tunnelling was helped with the protective plastic of a spinal block needle (Fig. 1[H-I]).
(A) 3D Trachea. (B) and (C) ETT placement in the 3D trachea. (D) Sealing the distal exit of the trachea with paper tape. (E) Fastening the trachea with foam adhesive tape. (F) Connection of ETT with manual air pump. (G) Infiltration of pork belly subcutaneous tissue with artificial blood. (H) and (I) Tunnelling of the pork belly with the help of the dural puncture needle protector. (J) Placement of iv infusion set connected to artificial blood and to the pressurizer. (K) Final result.
To evaluate the realism of the RCT model, with changes performed, five surgeons expert in cricothyroidotomy (two ear-nose-throat and three thoracic surgeons) participated in the study. They performed the technique in the model described and in a commercial dry model (Life/form® Cricothyrotomy Simulator 1082 Nasco, Fort Atkinson, Wisconsin) and score out 10 seven items regarding the technique.
To assess the model usefulness in a realistic scenario and with the aim of training cricothyrotomy in its clinical context, we integrated the phantom into a simulation scenario of CICO.
The programme SimMon® installed on an iPad® and remotely controlled by an iPhone® was used for simulating vital signs. Eleven participants to the simulation received the DA algorithms and briefing before they entered in the realistic simulation scenario to solve a CICO case by performing a cricothyrotomy with surgical technique upon the assembled model. The participants entered in teams of an anaesthesiologist and a ICU nurse. Simulation scenario was designed in the template used by us.5 Participants completed a survey on the phantom fidelity characteristics (Table 1).
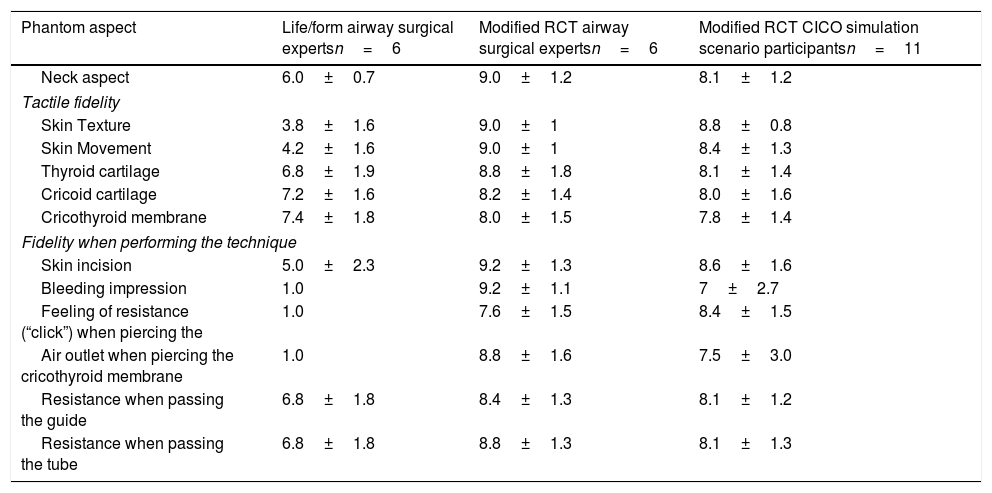
Assessment of the technical characteristics of the Life/form® and modified RCT by airway surgical experts and modified RCT by CICO simulation scenario participants. Assessment of modified RCT ultrasound images. Each item was rated on a 1 to 10 scale. Results are presented as mean±standard deviation.
| Phantom aspect | Life/form airway surgical expertsn=6 | Modified RCT airway surgical expertsn=6 | Modified RCT CICO simulation scenario participantsn=11 |
|---|---|---|---|
| Neck aspect | 6.0±0.7 | 9.0±1.2 | 8.1±1.2 |
| Tactile fidelity | |||
| Skin Texture | 3.8±1.6 | 9.0±1 | 8.8±0.8 |
| Skin Movement | 4.2±1.6 | 9.0±1 | 8.4±1.3 |
| Thyroid cartilage | 6.8±1.9 | 8.8±1.8 | 8.1±1.4 |
| Cricoid cartilage | 7.2±1.6 | 8.2±1.4 | 8.0±1.6 |
| Cricothyroid membrane | 7.4±1.8 | 8.0±1.5 | 7.8±1.4 |
| Fidelity when performing the technique | |||
| Skin incision | 5.0±2.3 | 9.2±1.3 | 8.6±1.6 |
| Bleeding impression | 1.0 | 9.2±1.1 | 7±2.7 |
| Feeling of resistance (“click”) when piercing the | 1.0 | 7.6±1.5 | 8.4±1.5 |
| Air outlet when piercing the cricothyroid membrane | 1.0 | 8.8±1.6 | 7.5±3.0 |
| Resistance when passing the guide | 6.8±1.8 | 8.4±1.3 | 8.1±1.2 |
| Resistance when passing the tube | 6.8±1.8 | 8.8±1.3 | 8.1±1.3 |
| Fidelity when applying ultrasound | Modified RCT ultrasound expertsn=2 |
|---|---|
| Subcutaneous skin and tissue | 7.5±0.5 |
| Transverse thyroid cartilage | 7.5±0.5 |
| Transverse cricoid cartilage | 8.5±0.5 |
| Transverse cricothyroid membrane | 7.5±0.5 |
| Sagittal thyroid cartilage | 7.5±0.5 |
| Sagittal cricoid cartilage | 7.0±0.5 |
| Sagittal cricothyroid membrane | 7.5±0.5 |
RCT: REAL CRIC Trainer. CICO: can’t intubate can’t oxygenate.
Experts and participants assessed the phantom aspect, tactile fidelity, fidelity when performing the technique with a numerical rating scale from 1 to 10.
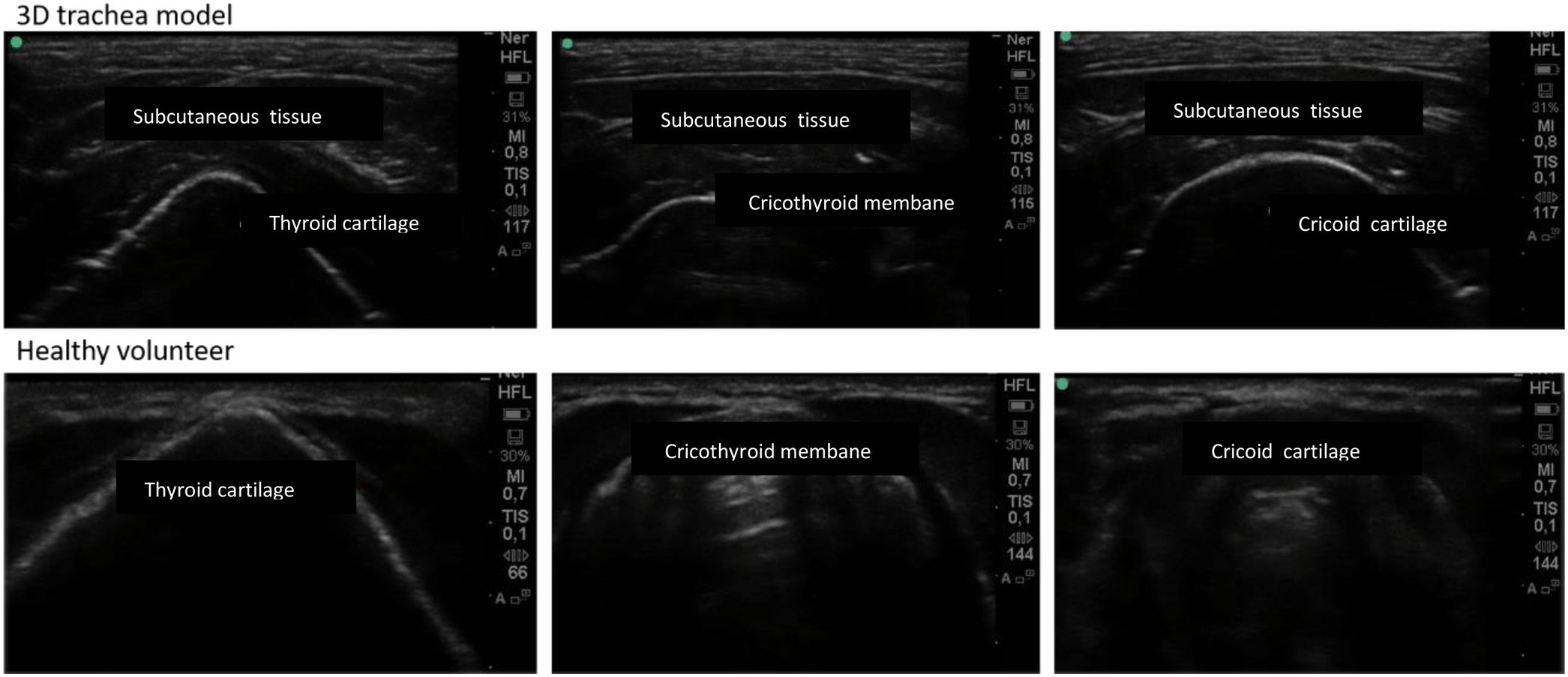
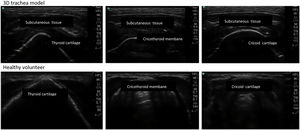
Ultrasonography application in the modified RCT modelUltrasonography was performed with the probe in the longitudinal and transverse plane visualizing the thyroid cartilage, cricothyroid membrane and cricoid cartilage on the model and in a volunteer among the simulation team members. The images obtained were recorded for later comparison. Two ultrasonography experts evaluated the images with a numerical rating scale from 1 to 10.
The sample size was determined by the nature of voluntary participation, so no formal sample size calculation was done. Descriptive statistics (mean value and dispersion by SD) was performed using Statistical Package for Social Sciences version 22.0 (SPSS, Chicago, IL).
ResultsThe bleeding when the skin is cut and the bubbling when the airway is reached were valued as a realistic experience not detectable in the dry model. Table 1 shows the results of the expert's evaluation.
Six anaesthesiologists and five nurses specialized in intensive care, the relevance of the workshop for daily practice, its approach and its development was rated 9.8±0.7 and the debriefing 9.9±03. All participants would recommend the workshop to a co-worker and would do it again. The evaluation of the phantom is shown in Table 1.
The modified RCT model were considered as high fidelity with respect those in volunteers, regarding to the images obtained by ultrasounds (Fig. 2, Table 1).
DiscussionThe adaptation that we carried out with the model RCT4 was better valued than the pre-existing dry traditional model, it allows to identify anatomical structures both by palpation and ultrasounds, achieved a high level of acceptance by the participants, besides, it allowed training non-technical skills, due to the contextualization of the model in a clinical setting.
Clinical simulation fills the gap allowing the repeated practice of techniques and their contextualization.
There are several approaches for cricothyrotomy, the percutaneous and the surgical technique.6 A systematic review could not demonstrate the superiority of the techniques.7 The surgical technique was considered superior in a pre.vious meta-analysis8 in The Fourth British National Survey and likewise in the Heymans et al.9 the surgical technique was also considered superior. The latest guidelines of the Difficult Airway Society in 201510 recommend surgical cricothyrotomy due to its high success rate of 100% compared to 67% of percutaneous techniques with thick cannula and 37% using the narrow cannula.
Multiple phantoms have been described for performing cricothyrotomy, from low cost and low fidelity models like the one described by Aho et al.11 built entirely from reusable materials, to high fidelity models using commercial simulators. Friedman et al.12 compared the impact of a low fidelity model with a high fidelity one and did not find differences for the acquisition of technical skills. Katayama et al.13 also found no differences in the acquisition of psychomotor skills comparing a low and high fidelity models. Takayesu et al.14 compared clinical cadaver versus mannequin simulation and pig trachea, and in this case the participants valued fidelity as a fundamental aspect of training.
From our point of view, the RCT with the modifications applied, becomes a useful low-cost and high realistic model, well suited for being integrated into a clinical simulation for training emergent cricothyrotomy. The semi-automation of air and blood outlet, allowing the instructor to be away from the participant gives realism to the scenario.
The usefulness of the model in a realistic scenario of CICO was evaluated almost at the highest rating. Contextual experience in realistic simulation scenarios allows a broader view, providing psychomotor training but also on non-technical skills such as decision making, communication abilities, multidisciplinary collaboration and leadership in a safe environment. The model was fully integrable in a realistic simulation scenario.
Despite our satisfactory experience in the model realism and in its performance to train emergent cricothyrotomy, the limited number of both training participants and experts, does not allow go further in expanding the usefulness for other groups. Nevertheless the data from this study allow us to consider this model for a more effective training than we previously did and encourages us to continue evaluating this model with more participants and by other groups.
The possibility of using the model for training cricothyroid membrane identification by ultrasonography is an aspect to highlight and enhance. Cricothyroid membrane palpation has only a 62% success rate13 and in obese patients and women the rate could be even lower. Echography increases the possibility of correct localization15 by up to 5.6 times.14 The use of ultrasounds could be included in the safety checklist for the management of the anticipated difficult airway.16
Our study has some limitations as the small sample for convenience of participants, the expert group was also limited but they were those in our hospital that had a high competence in performing the procedure. Likewise the model was only used to perform surgical cricothyrotomy and it cannot be stated whether it is also suitable for teaching percutaneous modalities. The most important limitation of the model is that it does not allow the detection of complications such as perforation of the posterior part of the trachea, oesophageal perforation or pneumothorax. However, it does allow measurement of the technique's time of completion and the global success with endotracheal tube placement in the trachea.
In conclusion, the REAL CRIC Trainer model with the described modifications is superior to dry model available on market according to surveys conducted, its integration into a simulation scenario is feasible and allows participants to acquire technical and non-technical skills for performing an urgent cricothyrotomy. The fidelity of the structure's images obtained by ultrasonography makes the model useful for training this skill.
Availability of data and materialsThe data that support the findings of this study will be available by request to the corresponding author upon reasonable request.
Ethics approval and consent to participateIt was submitted to the Ethics & Research Committee of Hospital Clinic de Barcelona and exemption was obtained (n° 12/2020).
FundingThe authors received no financial support for the research,
AuthorshipAll authors contributed to the study conception and design. The study design was performed by AC and CI. AC and CI have drafted the manuscript protocol. Participant recruitment, acquisition, analysis and interpretation of data will be performed by AC, CI, CG, LGL, VV, JP and RB have substantively revised the different contributions of all the authors and collaborated with the structure of this study and submission. All authors read and approved the final version.
Conflicts of interestThe authors declare no conflict of interest in relation to this manuscript.
The authors acknowledge valuable collaborations with the study to ear-nose-throat and thoracic surgeons.