The knowledge of COVID-19 and the recommended preventive measures for controlling the disease have been widely studied in the general population, but little is known about whether the University workers as educators and transmitters of knowledge have appropriate knowledge and take preventive measures for COVID-19. This study aims to analyze the knowledge of COVID-19 and the recommended preventive measures in university workers, to identify groups according to the preventive practices they adopt, and to analyze the factors associated with these practices.
Material and methodsA cross-sectional study was conducted on 677 university workers in the University of Cádiz, Spain. A questionnaire with sociodemographic variables, housing, health conditions, knowledge of COVID-19 and preventive measures were administered. The information was collected between 8th and 22nd April, 2020. A cluster analysis was performed to identify subgroups depending on the preventive measures. Associated factors were tested with binary logistic regression.
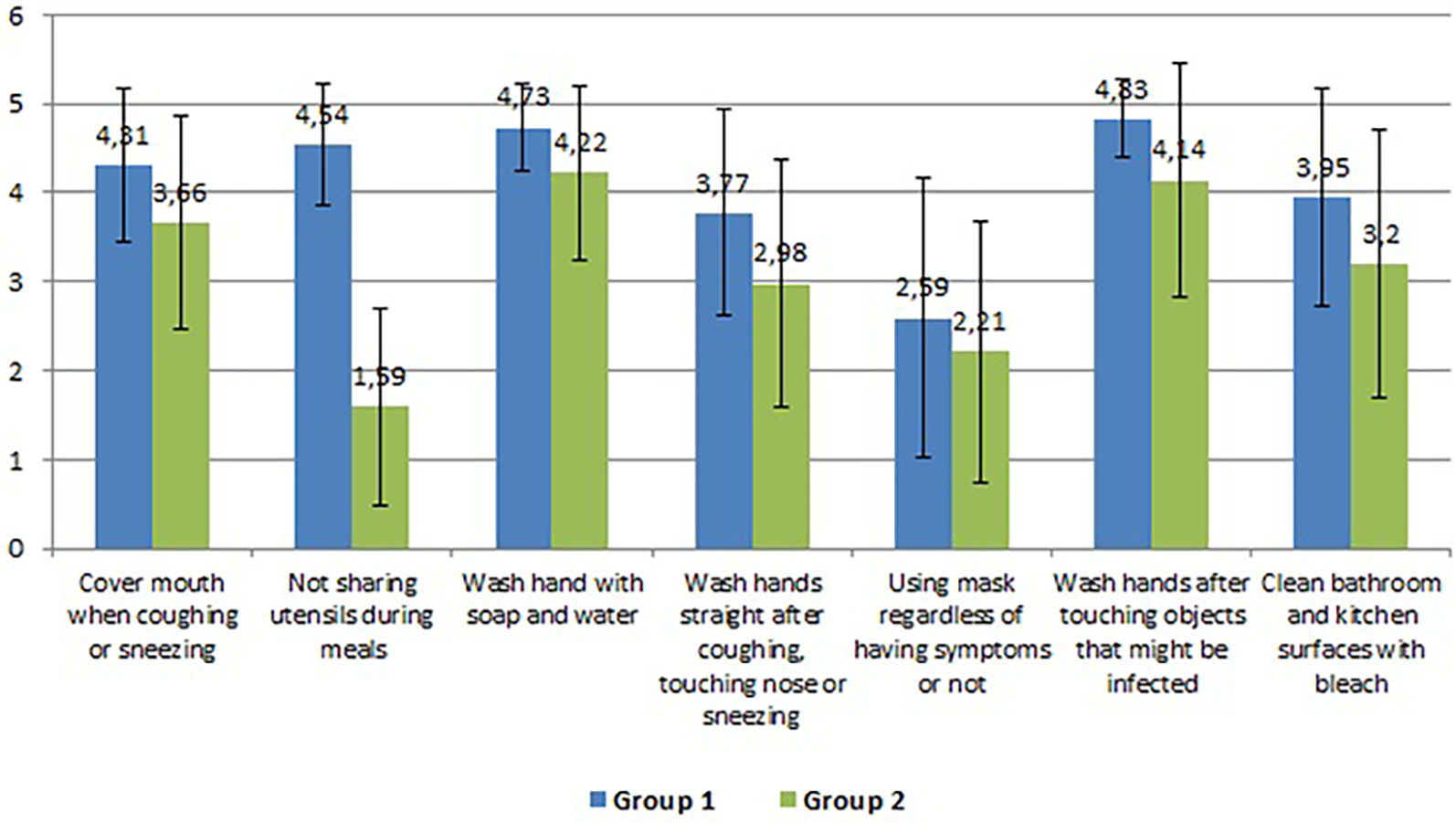
ResultsTwo groups were identified. Group 1 included 513 subjects who took preventive measures most frequently (means 2.59-4.83). Group 2 included 164 subjects who took preventive measures less frequently (means 1.59-4.22). Men (OR=1.39), the Teaching and research personnel (OR=1.49) and individuals with a chronic illness (OR=1.60) were more likely to belong to the group 2. Those with more knowledge about isolation prevention (OR=0.167) and early treatment (OR=0.665) were more likely to belong to group 1.
ConclusionIn order to reduce the transmission of the disease, it is necessary to promote the knowledge and use of preventive measures among the group of individuals identified as less engaged in preventive measures.
El COVID-19 y las medidas preventivas recomendadas para su control han sido ampliamente estudiados en la población en general. Sin embargo, poco se sabe sobre si los trabajadores universitarios como educadores y transmisores de conocimiento tienen los conocimientos adecuados y toman las medidas preventivas adecuadas. Este estudio tiene como objetivo analizar el conocimiento sobre el COVID-19 y las medidas preventivas recomendadas en trabajadores universitarios, así como, identificar grupos según las prácticas preventivas que adopten y analizar los factores asociados a estas prácticas.
Material y métodosSe realizó un estudio transversal en 677 trabajadores universitarios de la Universidad de Cádiz, España. Se administró un cuestionario (del 8 al 22 de abril) que recogía variables sociodemográficas, sobre su vivienda, condiciones de salud, conocimiento del COVID-19 y medidas preventivas. Se realizó un análisis de conglomerados para identificar subgrupos en función de las medidas preventivas. Los factores asociados se probaron con regresión logística binaria.
ResultadosSe identificaron dos grupos. El grupo 1 incluyó a 513 sujetos que tomaban medidas preventivas con mayor frecuencia (medias 2,59-4,83). El grupo 2 incluyó a 164 sujetos que tomaron medidas preventivas con menor frecuencia (medias 1,59-4,22). Los hombres (OR=1,39), el Personal Docente e Investigador (OR=1,49) y las personas con alguna enfermedad crónica (OR=1,60) tenían mayor probabilidad de pertenecer al grupo 2. Los que tenían más conocimientos sobre prevención del aislamiento (OR=0,167) y el tratamiento temprano (OR=0,665) tenían más probabilidades de pertenecer al grupo 1.
ConclusiónPara reducir la transmisión de la enfermedad es necesario promover el conocimiento y uso de medidas preventivas entre el grupo de individuos identificados como menos comprometidos con las medidas preventivas.
The coronavirus disease 2019 (COVID-19) is an illness caused by a novel coronavirus called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), first identified in Wuhan City, Hubei Province, China.1 The initial lack of knowledge of the causal agent, of its transmission mechanisms, of effective ways of controlling it and the high numbers of infected people resulted in the WHO declaring a pandemic on 11th March 2020. As of October 2021, the number of infected people in Spain has reached 4.97 million, while 86,701 people have died.2
At the beginning of the pandemic, based on the knowledge acquired from other pandemics, public health experts established recommended guidelines to prevent the spreading of the disease. Basically, these recommendations were the self-isolation of patients and their contacts, hand hygiene, wearing masks and social distancing.3,4 However, these measures have undergone changes as our understanding of the disease increased.
The initial lack of knowledge and the misleading information provided by the media and social networks have resulted in many problems and uncertainty among the population, which has led to misunderstandings about COVID-19 among both the general population and specific groups,5,6 and consequently to more infections and deaths. Studies into this topic performed in healthcare professionals show that a lack of knowledge of the disease may lead to a delay in its diagnosis and treatment being given, resulting in an increase in transmissions and the principle of zero infection-risk and community transmission being unachievable,7
Furthermore, there are factors that lead to differences in how the population follow the recommended preventive measures. There is evidence that gender and educational level are associated with the prevention of COVID-19, in that men and individuals with a lower level of education take preventive measures less frequently.8,9 Likewise, it has been reported that people with chronic diseases such as allergic or immune diseases are more likely to be adherent to preventive behaviors.10 In this vein, several authors have shown that having adequate knowledge during pandemics leads people to consider themselves at risk of infection, which may in turn lead them to adopt preventive behavior.11–13
In view of the importance of having the appropriate knowledge and information about the pandemic, and identifying the characteristics associated with taking preventive measures less frequently, it was considered important to analyze these aspects with regard to university workers. There is a lack of studies about the impact of COVID-19 in this sector, despite the role played by university workers as educators and transmitters of knowledge to their students, and by the administration and services workers, who are responsible for organizational measures. To this end, we proposed to analyze the knowledge of COVID-19 and the recommended preventive measures for controlling the disease adopted by the workers of the University of Cádiz three and a half weeks after the onset of the pandemic. As a secondary aim we proposed to establish groups among the university workers according to the preventive practices they adopted, and to analyze the sociodemographic and clinical variables associated with these practices.
Material and methodsA cross-sectional, descriptive study was conducted in which the study population was the personnel included in the census of the University of Cádiz in March 2020, including both research and teaching personnel (RTP) (2,047) and administration and services personnel (ASP) (842). Having the complete census made it possible to gain access to all the workers. The final study sample consisted of 677 people.
Information was collected between 8th and 22nd April, 2020 after three and a half weeks of lockdown by means of an online survey prepared with the Google Form platform. The study population was contacted via the university e-mail address that is provided to all of the workers.
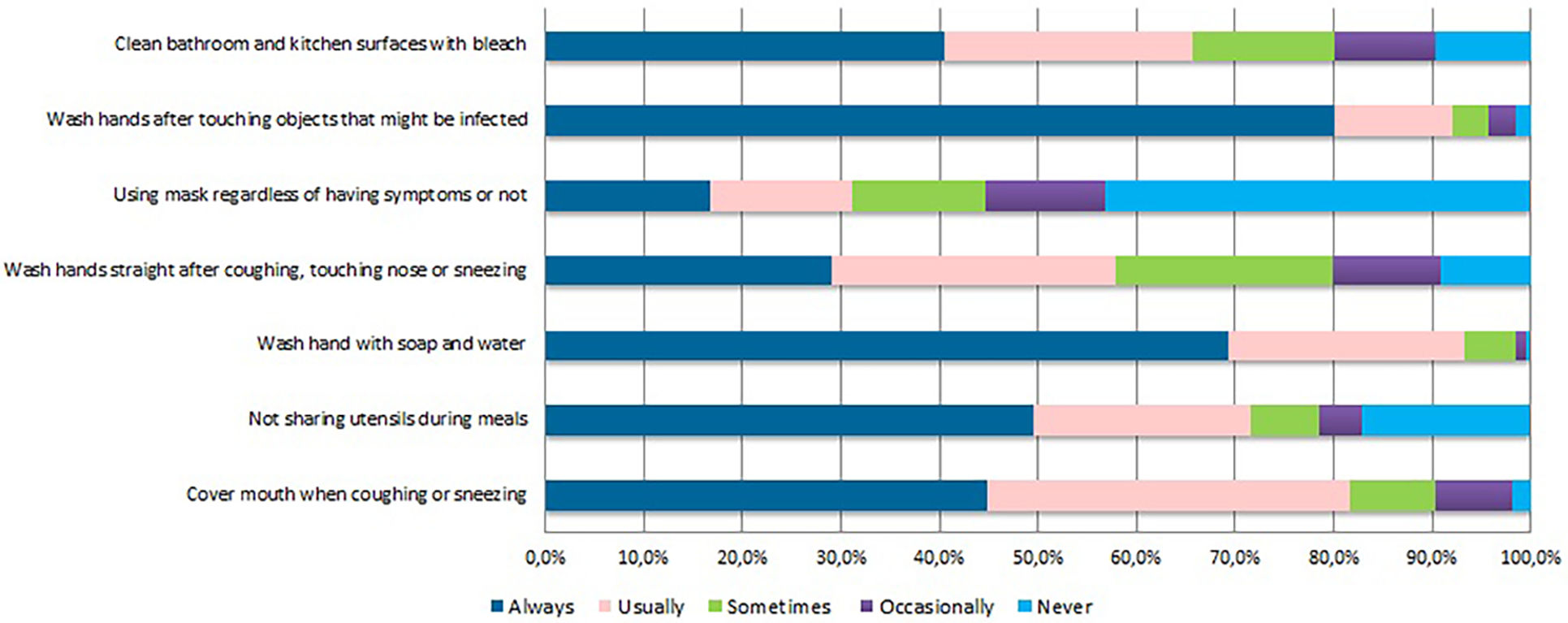
The data collection questionnaire was divided into six blocks that included information about sociodemographic data, knowledge of COVID-19, clinical aspects, impact on daily life, impact on work and economy, and emotional aspects. The following information was used for the aims of this study: gender, age, marital status, labor sector (RTP: Research and Teaching Personnel; ASP: Administration and Services Personnel), professional category (for RTP: Predoctoral contract, Post-doctoral Research Assistantship/Fellowship, Assistant or Associate Lecturer, Lecturer, Senior Lecturer or Reader, Associate Professor, Professor or other; for ASP: Group I (best working conditions) to Group IV (worst working conditions)), information about their household (income, number of cohabitants) and size and availability of open space in the home; information about their general health status, history of chronic illness, presence, origin and state of chronic pain compared with before the state of alarm and situation regarding COVID-19 (having the virus and/or contact with it) (Table 1). Furthermore, several items were included to evaluate the subjects’ knowledge of COVID-19 in which they had to answer true or false (Table 2). Likewise, questions were included about seven actions related with the preventive measures taken against COVID-19 (covering their mouth when coughing, avoiding sharing utensils, hand washing, hand washing after coughing and sneezing, using masks, hand washing after touching contaminated objects, and cleaning bathroom and kitchen surfaces with bleach), which were evaluated on a Likert scale from 1 (never) to 5 (always) (Fig. 1).
Sociodemographic and clinical characteristics of the sample (N=677).
| Sociodemographic characteristics | |
|---|---|
| Variable | N (%) |
| Gender (N=676) | |
| Male | 337 (49.9%) |
| Female | 339 (50.1%) |
| Age (Years) (N=666) | Mean (SD) |
| 48.75 (10.51) | |
| Marital status (N=676) | |
| Married or in a relationship | 491(72.6%) |
| Widow(er) | 52 (7.7%) |
| Divorced or separated | 126 (18.6%) |
| Single | 7 (1%) |
| Educational Level (N=674) | |
| Primary | 3 (0.4%) |
| Secondary | 66 (9.8%) |
| University | 605 (89.8%) |
| Labour sector | |
| RTP | 423 (62.5%) |
| ASP | 254 (37.5%) |
| Professional category (RTP) (N=411) | |
| Predoctoral contract | 21 (5.1%) |
| Post-doctoral Research Assistantship/Fellowship | 12 (2.9%) |
| Assistant or Associate Lecturer | 98 (23.8) |
| Lecturer | 23 (5.6%) |
| Senior Lecturer or Reader | 138 (33.6) |
| Associate Professor | 38 (9.2) |
| Professor | 64 (15.6) |
| Other | 17 (4.1) |
| Area of knowledge (RTP) (N=423) | |
| Arts and Humanities | 68 (16.1%) |
| Science | 119 (28.1%) |
| Health sciences | 51 (12.1%) |
| Social and legal sciences | 104 (24.6%) |
| Engineering and architecture | 81 (19.1%) |
| Professional category (ASP) (N=206) | |
| Group I (best conditions) | 33 (16.0%) |
| Group II | 40 (19.4%) |
| Group III | 85 (41.3%) |
| Group IV (worst conditions) | 48 (23.3%) |
| Household income level (per month) (N=669) | |
| From €500 to €1499 | 83 (12.4%) |
| From €1500 to €2999 | 294 (43.9%) |
| From €3000 to €4999 | 219 (32.7%) |
| €5000 or more | 73 (10.9%) |
| Housing | |
| Number of people living with you (including yourself) (N=672) | |
| 1 | 77 (11.5%) |
| 2 | 214 (31.8%) |
| 3 | 154 (22.9%) |
| 4 | 175 (26.0%) |
| 5 or more | 52 (7.7%) |
| Mean (SD) | 2.9 (1.27) |
| Children under 14 years old living with you (N= 669) | |
| 0 | 490 (73.5%) |
| 1 | 89 (13.3%) |
| 2 | 72 (10.8%) |
| 3 or more | 16 (2.4%) |
| Mean (SD) | 0.43 (0.81) |
| Number of dependent people under your care (over 14 years old) (N= 659) | |
| 0 | 521 (79.5%) |
| 1-2 | 121 (18.5%) |
| 3 or more | 13 (2%) |
| Size of your home (N=674) | |
| Up to 49 m2 | 20 (3%) |
| 50 - 89 m2 | 242 (35.9%) |
| 90 - 129 m2 | 250 (37.1%) |
| 130 m2 or more | 162 (24%) |
| Does your home have open areas like a garden, balcony, patio or porch? (N=674) | |
| Yes | 395 (58.6%) |
| No | 279 (41.4%) |
| Habits | |
| Tabaco consumption | |
| Much more than before | 5 (0.7%) |
| More than before | 19 (2.8%) |
| Same as before | 71 (10.5%) |
| Less than before | 10 (1.5%) |
| Much less than before | 13 (1.9) |
| I never do it | 559 (82.6%) |
| Alcohol consumption | |
| Much more than before | 11 (1.6%) |
| More than before | 61(9%) |
| Same as before | 261(38.6%) |
| Less than before | 81(12%) |
| Much less than before | 67(9.9%) |
| I never do it | 196(29%) |
| Health conditions | |
| Variable | N (%) |
| Health status at the time of the survey: | |
| Much worse than before the lockdown | 6(0.9%) |
| Worse than before the lockdown | 96(14.2%) |
| Same as before the lockdown | 545(80.5%) |
| Better than before the lockdown | 30(4.4%) |
| Much better than before the lockdown | 0(0.0%) |
| History of chronic disease | |
| Yes | 224(33.1%) |
| No | 453(66.9%) |
| Chronic diseases (N=224) | |
| High blood pressure | 88(39.3%) |
| Diabetes | 29(12.9%) |
| Cardiovascular disease | 28(12.5%) |
| Respiratory disease | 62(27.7%) |
| Cancer | 11(4.9%) |
| Immune disease | 30(13.4%) |
| Presence of chronic pain | |
| Yes | 94(13.9%) |
| No | 583(86.1%) |
| What is the main cause of that pain? (N=93) | |
| I don't know. | 5(5.4%) |
| Arthrosis | 15(16.1%) |
| Back pain | 26(28%) |
| Migraine or other chronic headaches | 8(8.6%) |
| Rheumatoid arthritis | 2(2.2%) |
| Sciatica | 4(4.3%) |
| Neck contracture or problems | 9(9.7%) |
| Painful shoulder | 2(2.2%) |
| Fibromyalgia | 3(3.2%) |
| Diabetic neuropathy or other neuropathy | 1(1.1%) |
| Other causes (tendinitis, spondylitis, muscular dystrophy, etc.) | 18(19.4%) |
| Intensity of pain during the lockdown | |
| Much worse than before the lockdown | 8(8.6%) |
| Worse than before the lockdown | 31(33.3%) |
| Same as before the lockdown | 46(49.5%) |
| Better than before the lockdown | 8(8.6%) |
| Much better than before the lockdown | 0(0%) |
| Having or contact with COVID-19 | |
| Variable | N (%) |
| Have you been tested to see if you have been infected by COVID-19? | |
| No | 674(99.6%) |
| Yes, with negative result | 3(0.4%) |
| Yes, with positive result | 0(0%) |
| Yes, waiting for result | 0(0%) |
| Have you required hospital admission during the state of alarm? (N=676) | |
| Yes, for COVID-19. | 0(0%) |
| Yes, for reason other than COVID-19. | 5(0.7%) |
| No | 671(99.3%) |
| Have you been in physical contact with anyone with a confirmed COVID-19 diagnosis without any personal protection (gloves, mask)? (N=674) | |
| Yes | 12(1.8%) |
| No | 662(98.2%) |
| How many people among family/friends have tested positive for COVID-19? (N=671) | |
| 0 | 554(82.6%) |
| 1-2 | 89(13.3%) |
| 3 or more | 28(4.1%) |
| Are you living with anyone during the state of alarm that has tested positive for COVID-19? | |
| No | 676(99.9%) |
| Yes, with one person. | 1(0.1%) |
| Yes, with more than one person. | 0(0%) |
| During the state of alarm, are you living with anyone over the age of 60 or with a chronic illness considered to be at risk of infection? | |
| Yes | 168(24.8%) |
| No | 509(75.2%) |
Knowledge of COVID-19 (N=677).
| Knowledge of Transmission pathways of COVID-19 | ||
|---|---|---|
| Questions | N (%) | Correct Answer |
| Eating wild animals or contact with them could cause infection with COVID-19. | ||
| True | 230(34%) | False |
| False | 239(35.3%) | |
| DK/DA | 208(30.7%) | |
| People with COVID-19 without a fever cannot infect other people. | ||
| True | 89(13.1%) | False |
| False | 573(84.6%) | |
| DK/DA | 15(2.2%) | |
| COVID-19 is spread through the respiratory droplets of infected individuals. | ||
| True | 641(94.7%) | True |
| False | 9(1.3%) | |
| DK/DA | 27(4%) | |
| Knowledge of clinical signs of COVID-19 | ||
| The main symptoms of COVID-19 are fever, dry cough and breathing difficulties. | ||
| True | 675(99.7%) | True |
| False | 1(0.1%) | |
| DK/DA | 1(0.1%) | |
| Nasal congestion, runny nose and sneezing are less common in COVID-19 than in a common cold. | ||
| True | 517(76.4%) | True |
| False | 63(9.3%) | |
| DK/DA | 97(14.3%) | |
| Although there is no effective cure for COVID-19, the early treatment of the symptoms can help most patients to recover. | ||
| True | 429(63.4%) | True |
| False | 97(14.3%) | |
| DK/DA | 151(22.3%) | |
| Only the elderly, people with chronic illnesses or the obese are at risk of serious illness. | ||
| True | 123(18.2%) | False |
| False | 523(77.3%) | |
| DK/DA | 31(4.6%) | |
| Knowledge of prevention and control of COVID-19 | ||
| The use of surgical masks in the general population prevents infection with COVID-19. | ||
| True | 435(64.3%) | True |
| False | 144(21.3%) | |
| DK/DA | 98(14.5%) | |
| It is not necessary for children and teenagers to take measures to prevent infection with COVID-19. | ||
| True | 10(1.5%) | False |
| False | 656(96.9%) | |
| DK/DA | 11(1.6%) | |
| Crowded places (stations and public transport) should be avoided to prevent infection. | ||
| True | 665(98.2%) | True |
| False | 10(1.5%) | |
| DK/DA | 2(0.3%) | |
| The self-isolation of people infected with COVID-19 is an effective way to stop the virus from spreading. | ||
| True | 671(99.1%) | True |
| False | 4(0.6%) | |
| DK/DA | 2(0.3%) | |
| People that come into contact with anyone infected with COVID-19 must self-isolate immediately for 14 days. | ||
| True | 599(88.5%) | True |
| False | 36(5.3%) | |
| DK/DA | 42(6.2%) | |
A descriptive analysis was performed of all the data obtained, showing the absolute and relative frequencies of the qualitative variables and the mean values with their corresponding standard deviations in the case of quantitative variables.
To classify the participants of the study according to how they followed preventive measures against COVID-19, a cluster analysis was performed, the classification variables being the seven preventive measures the subjects were asked about in the questionnaire. They were considered quantitative variables with values from 1 to 5, a higher score indicating a greater frequency of engaging in the preventive measure. A hierarchical method was used for this analysis based on measuring the squared Euclidean distance and Ward’s method. A dendrogram and sedimentation graph were used to select the number of clusters.
Then, the Mann-Whitney U test was used to compare the mean scores of each preventive measure between the groups obtained in the cluster analysis. Subsequently, a stepwise backward binary regression model was constructed to determine the factors associated with the sub-groups previously identified. The dependent variable was the clusters identified and the independent variables were the sociodemographic, clinical and knowledge variables described above. The criteria used for selecting the variables included in the model were clinical and statistical (significance observed in the bivariate analysis, p<0.05: data not shown).
The analyses were performed with the IBM-SPSS-Statistics-v24 and Rv.3.5.1 statistical tools.
Ethical considerationsThe study was conducted in agreement with the international ethical criteria established in the Helsinki Declaration. All the information collected was confidential in agreement with Organic Law 3/2018 on data protection and guarantee of digital rights. In addition, all the data were collected and used anonymously. The workers were informed of the nature and aims of the study, and were asked to voluntarily sign the informed consent, guaranteeing their anonymity during the whole process. The University of Cádiz provided its consent to conduct this survey, ensuring adherence to ethical standards.
ResultsAmong the 677 subjects surveyed, 50.1% were women and the overall mean age was 48.75 years (SD=10.51). Most of the people reported being married or in a relationship (72.6%). Likewise, most referred to having a university education (89.9%) (Table 1).
Research and teaching personnel (RTP) constituted 62.5% of the respondents, and regarding the area of knowledge in which they worked, 28.1% were in sciences, followed by social sciences (24.6%) and engineering and architecture (19.1%). Administration and services personnel (ASP) constituted 37.5% of the sample, 41.3% of whom belonged to Group III (Table 1).
Regarding the socio-economic characteristics of the respondents, 32.7% stated that the net household monthly income was between €3000 and €4999, and 31.9% reported that their household comprised two people. Among all of the respondents, 37.1% reported living in a home of between 90 and 129 m2, and 58.6% indicated that their homes had an outdoor space such as a garden, balcony or patio (Table 1).
As for the habits of the people interviewed during the state of alarm, the great majority did not smoke tobacco (82.6%) and only 3.5% smoked more o much more tobacco than before the state of alarm. The 10.6% consumed more o much more alcohol than before the state of alarm and 38.6% consumed the same as before. Regarding the health status of the respondents, most (80.5%) stated that their health status was the same as before the state of alarm, although 15.1% indicated that their health was worse or much worse than before (Table 1). A total of 33.1% had a history of chronic illness such as high blood pressure (39.3%), respiratory disease (27,7%) or cardiovascular disease (12.5%); meanwhile, 13.9% reported suffering from chronic pain, the most common being back pain (28%), followed by arthrosis (16.1%). It is of note that 41.9% of the respondents that referred to chronic pain considered their pain to be worse or much worse than before the state of alarm (Table 1).
Regarding symptoms related with COVID-19, 63.5% mentioned having had at least one symptom, the most frequent being headache (45%) and tiredness (30.3%) (Data not shown). However, only 0.4% had taken the test for COVID-19, obtaining a negative result. A total of 1.8% said they had been in contact with someone with a confirmed diagnosis of COVID-19, and 17.4% reported having a relative or friend with the illness (Table 1).
In the analysis of knowledge of COVID-19, the aspects related with the main symptoms produced by the virus were found to be the most known (99.7%), followed by the obligation for infected people to self-isolate (99.1%) and avoiding crowded places (98.2%). The least known aspects were those related with routes of transmission, as 34% of the respondents answered that eating wild animals or contact with them could result in infection, and 13.1% believed that people without a high temperature cannot spread the virus. A greater lack of knowledge was observed (14.5%) in relation to the use of surgical masks to prevent infection, and about the fact that the early treatment of the symptoms can help most patients in their recovery (22.3%) (Table 2).
Finally, the preventive measures that the respondents took most of the time or always were “hand washing with soap and water” (93.2%) and “covering your mouth when coughing and sneezing” (81.7%). Of note is that 55.1% of the respondents used a mask only occasionally or never, and 21.4% shared utensils during meals (Fig. 1).
Groups of respondents identified according to preventive measures adoptedFrom the cluster analysis, 2 groups were identified. Group 1 included 513 subjects who took preventive measures most frequently, the mean values for the seven measures analyzed ranging from 2.59 to 4.83 (Fig. 2). Group 2 included 164 subjects who took preventive measures less frequently, the mean values ranging between 1.59 and 4.22 (Fig. 2).
An analysis of the factors related to these 2 sub-groups revealed that men (OR=1.39), the RTP (OR=1.49) and the subjects with a history of chronic illness (OR=1.60) were more likely to belong to group 2 (took fewer preventive measures). However, those that gave the correct answer to the questions “The self-isolation of people infected with COVID-19 is an effective way of reducing the spread of the virus” and “Although there is no effective cure for COVID-19, the early treatment of symptoms can help most patients to recover”, were less likely to belong to group 2 (OR=0.167 and OR=0.665, respectively) (Table 3).
Associated factors with the sub-groups of subjects based on levels of prevention measures. Binary Logistic Regression Model. (N=676)
| B | OR(CI95%) | p | |
|---|---|---|---|
| Constant | 0.274 | 1316 | 0.762 |
| Sex | |||
| Men | 0.335 | 1.398(0.97;2.01) | 0.072 |
| Women* | |||
| Labour sector | |||
| RTP | 0.403 | 1.496(1.02;2.21) | 0.042 |
| ASP* | |||
| History of chronic illness | |||
| Yes | 0.472 | 1.603(1.12;2.32) | 0.012 |
| No* | |||
| The self-isolation of people infected with COVID-19 is an effective wayto stop the virus from spreading. | |||
| Correct | |||
| Incorrect* | -1.79 | 0.167(0.30;0.94) | 0.042 |
| Although there is no effective cure for COVID-19, the early treatment of the symptoms can help most patients to recover. | |||
| Correct | -0.408 | 0.665(0.46;0.96) | 0.028 |
| Incorrect* |
Dependent Variable: Groups of individuals according to levels of preventive measures. Group 1*, Group 2.
*Reference Category
Hosmer Lemeshow: Chi square= 2.065; p-value=0.979
This study analyses knowledge of COVID-19 and the preventive measures against this illness adopted by university workers. The results of the study highlight that the aspects that the respondents knew most about were those related with the main symptoms produced by the virus and the need for infected people to self-isolate. However, a noteworthy percentage of the university workers lacked knowledge about aspects related with how the virus is spread. Regarding preventive measures, the study highlights that hand washing with soap and water and covering your mouth when coughing and sneezing were the measures taken most frequently, while using masks and not sharing utensils during meals were the least respected. In addition, it was observed that men, the RTP group of professionals, subjects with a history of chronic illness, and those with less knowledge of matters such as isolation prevention and early treatment, were more likely to engage less frequently in preventive measures.
One result that stands out is the lack of knowledge of COVID-19 among the university workers, an explanation for which could be that the data was collected during the initial stage of COVID-19 in Spain, when knowledge of the virus and disease was very limited. These results are in the line with an earlier study conducted in Turkish adults,13 which reported inadequate knowledge and attitudes about COVID-19, as happened with previous infectious diseases such as SARS (Severe Acute Respiratory Syndrome) or MERS (Middle East Respiratory Syndrome).14,15 Another feasible explanation could be that the survey population did not work in healthcare. Several studies involving healthcare providers6 have shown that a high percentage of professionals have a good knowledge of COVID-19 (mean percentage: 75.8%), but that professionals from other sectors do not have knowledge of or understand communicable diseases and their mechanisms of action that justify the use of common preventive measures.
Compliance with preventive measures to successfully control diseases requires and is influenced by having the appropriate knowledge.16 Thus, as expected, many participants did not engage in preventive behavior against COVID-19 to protect themselves from the virus. The most frequently practiced preventive behaviors included hand washing with soap and water and covering your mouth when coughing or sneezing. Other studies conducted in other countries at the start of the pandemic reported that wearing a mask, not visiting crowded places and frequent hand washing were among the most practiced preventive behaviors.8,13 However, this study found that wearing a mask was not among the most frequently-used measures, although it is worth highlighting that their use was not obligatory at that time in Spain.
The study identified two groups according whether the subjects took the preventive measures explored to a greater or lesser extent, showing that men, the research and teaching group (RTP), subjects with a history of chronic illness and those who knew least about COVID-19 were more likely to take preventive measures less frequently.
In line with previous studies, male subjects were less likely to use preventive measures.8,17 However, contrary to our hypotheses, people with chronic diseases and from the RTP category were less likely to use preventive measures, despite RTP workers having a higher level of education, which has been related to better health awareness and health-related knowledge in the literature.18 However, the vast majority of the RTP had a positive perception of the illness (measured with The Brief Illness Perception Questionnaire (BIPQ), data not shown), which means a lower perceived risk. In this vein, previous research19 found that a higher perceived risk during the SARS outbreak was important in determining compliance with official advice. Related to patients with chronic illnesses, this has been shown20–22 to be associated with low health literacy. Low health literacy implies that these individuals have difficulty understanding health-related information holistically, influencing their behavior and the development of self-management skills, which is a significant predictor of COVID-19 awareness and preventive behavior,23 as our results show.
The strength of this study lies in the large sample recruited during a critical period, the early stage of the COVID-19 outbreak. Nevertheless, some limitations must be taken into account in this study. First, the information was gathered via email, which may contribute to some bias. Some authors have shown how obtaining information via e-mail could lead to casual answers to some questions due to disinterest or survey fatigue.24 Secondly, in the case of this study, the population was contacted via the university e-mail addresses, which did not guarantee that the answers obtained were representative by areas of knowledge or type of professional category. However, this data collection method allowed us to use a longer questionnaire than in telephone interviews, in which we could not have used validated scales. Finally, the data was collected after only three-and-a-half weeks of lockdown, a greater impact possibly being found at the end of the lockdown. However, the uncertainty of its duration and the lack of control could also have had an important impact. Additionally, at that specific moment of the Covid-19 pandemic, the majority of the population (not only the university population) lacked reliable information, since the information provided by the media and health and political authorities was sometimes inaccurate or contradictory. Thus, the results of this study could have be different if the information had been gathered later, when the knowledge of this disease had advanced considerably.
Concerning transferability, it is important to consider the context where this study was conducted: professionals of a Spanish university. With this in mind, we consider that the results from this study could be relevant for understanding the knowledge of COVID-19 or other infectious illnesses and prevention measures among professionals of other universities, since the consequences that they faced and the concerns that they have may be the same.
This study shows that at the beginning of the COVID-19-related lockdown, university workers lacked knowledge of COVID-19 and did not engage very frequently in preventive behavior. Men, research and teaching personnel, and individuals with a history of chronic illness were more likely to engage in preventive measures less frequently. Thus, it is necessary that the teaching of preventive measures focuses on these groups of individuals in order to reduce the transmission of the disease.
Declaration of Conflicting InterestsThe authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
FundingThe authors received no financial support for the research, authorship, and/or publication of this article.
The authors want to thank to all the university employees who agreed to participate in the study.