Practicing models for invasive procedure have proven useful in achieving better rates of success for physicians in training. Often, these models are not easy to get because of its expensive price. Radial artery cannulation is a common practice and its performance with ultrasonographic guidance has proven to be more efficient than traditional ways. We developed a low-cost practicing model that may aid physicians in training to master the ultrasound-guided radial artery cannulation technique and achieve better rates of success when performing this procedure.
MethodsUsing ordinary materials such as a piece of pork ham and rubber torniquets, we were able to build a 3-vessel artery model with pulsatile flow.
ResultsUltrasonographic imaging revealed a vessel-like material embedded inside the piece of ham. This material resembles an artery which can be punctured with an in-plane or out-of-plane technique and cannulated afterwards, either with a Seldinger or a modified Seldinger technique. Once cannulated, pulsatile flow can be obtained through the catheter used.
ConclusionOur model building time was 30 minutes, and its price doesn’t exceed more than $7.50 USD. This model can be used by physicians in training to practice the cannulation of a radial artery using ultrasonographic guidance.
Los modelos de práctica para procedimientos invasivos han probado ser útiles en mejorar las tasas de éxito de los médicos en entrenamiento que llevan a cabo tales procedimientos.
Frecuentemente, estos modelos son de difícil acceso debido a su elevado precio. La canulación de la arteria radial es una práctica común y la técnica con guía ultrasonográfica ha demostrado ser más eficiente que la técnica convencional. Desarrollamos un modelo de bajo costo que puede ayudar a los médicos en entrenamiento a perfeccionar ésta técnica y conseguir mejores tasas de éxito al realizar este procedimiento.
MétodosUtilizando materiales ordinaries como una pieza de jamón de cerdo y torniquetes huecos de hule, pudimos construir un modelo de simulación de 3 vasos arteriales con flujo pulsátil.
ResultadosLa ultrasonografía del modelo reveló que el material dentro del jamón tiene un gran parecido a una arteria radial. Este material tiene flujo pulsátil y mediante guía ultrasonográfica con técnica “En-plano” o “Fuera-de-plano” puede ser puncionado y canulado posteriormente ya sea con técnica Seldinger o Seldinger modificado y también permite observar el retorno de un flujo pulsátil a través de la cánula utilizada.
ConclusiónEl tiempo de construcción de nuestro modelo no excede los 30 minutos y el precio para hacerlo no asciende a más de $7.50 USD. Este modelo puede ser utilizado por personal de la salud en entrenamiento para practicar y perfeccionar la técnica de canulación radial con guía ultrasonográfica.
The use of ultrasound in medicine as a daily basis is today, a reality. In critical areas, it has proven useful in monitorization of the critically ill patient and a vital tool for invasive procedures.1 Several institutions recommend the use an ultrasound-guided technique for the insertion of a central venous catheter, since it has demonstrated to reduce the rate of mechanical complications and increase the success rate of the first attempt.1 Recommendations for the insertion of radial artery catheters do not defer significantly, and more than a few prospective studies have demonstrated that the use of an ultrasound guided technique in this scenario also provides a higher first-attempt success and a lower failure rates both in the critically ill and in the patient scheduled for cardiac catheterization.2–4
As for any other invasive procedure, achieving a successful radial artery access requires practice. In a sub-analysis of the SURF Trial which evaluated the outcomes of a transradial versus transfemoral approach and a standard versus ultrasound-guided technique, it was seen that the learning curve for radial arterial cannulation with ultrasound guidance required 50%-100% more procedures than for its femoral counterpart.5
Simulator and artificial models may provide a mean of achieving the experience needed to master this technique6 but the existing available models tend to be expensive, with prices exceeding $600.00 USD for models similar to the Blue Phantom Branched 4 Vessel Ultrasound Training Block (CAE Healthcare®, Sarasota, FL, USA). Because of this, authors around the world have created cheaper and simpler models that have demonstrated to be a reliable option for providing an enhancing teaching experience for central venous cannulation as well as for arterial catheter insertion, even with pulsatile models.7,8 Some of these models have proven to be cheap, with prices as low as € 9.0 and with a 40 minute construction time.7
The finding of these models published in medical literature motivated us to build one of our own, to let the residents at our institution practice the ultrasound-guided arterial cannulation procedure and shorten their learning curve. We developed a simple, feasible, reusable, pulsatile radial artery model with ordinary materials such as pork ham and latex rubber tourniquet tube, with pricing not exceeding $ 7.50 USD and a building time of not more than 30 minutes.
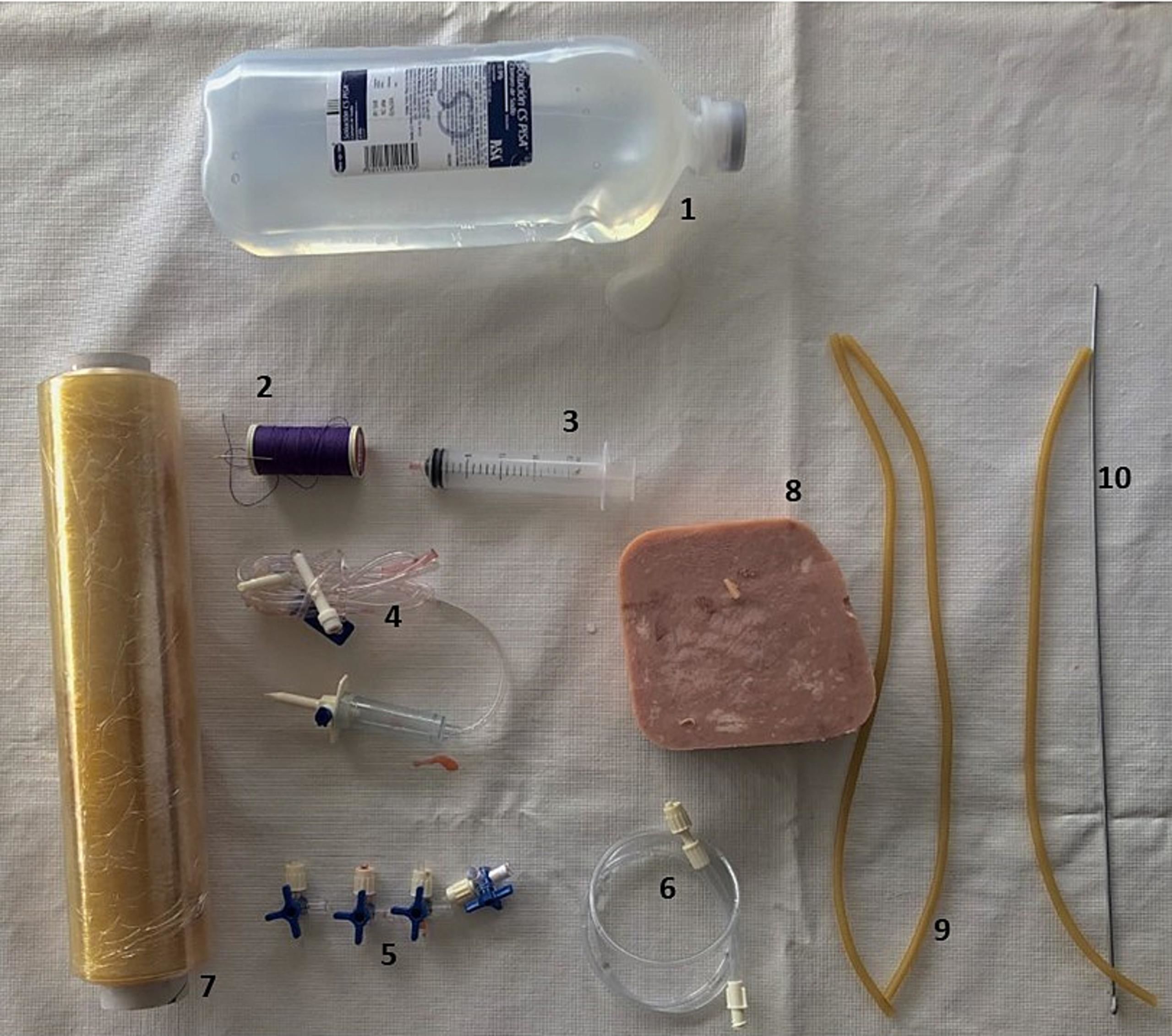
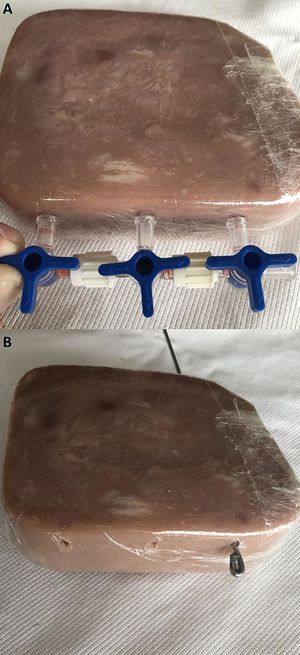
MaterialsThe central part of our model is a 500 grs. cubic piece of pork ham, which is an easily accessible and cheap material. The rest of the materials needed for its construction are depicted in Fig. 1 and consist of a cotton thread, a sewing needle, 20 ml syringe, 1 lt. solution bag, four 3-way stopcocks, plastic sealing wrap, 30 cm 1/8” aluminum wire, and an IV-line infusion kit with an extension.
Even though the mean radial artery size is 2.45 ± 0.54 mm, its diameter may be influenced by factors such as gender, previous medication, and chronic conditions in each patient.9 Because of this, we chose to use a 2.5 mm diameter latex rubber tourniquet tube, with 1 meter being more than enough for the building of the model.
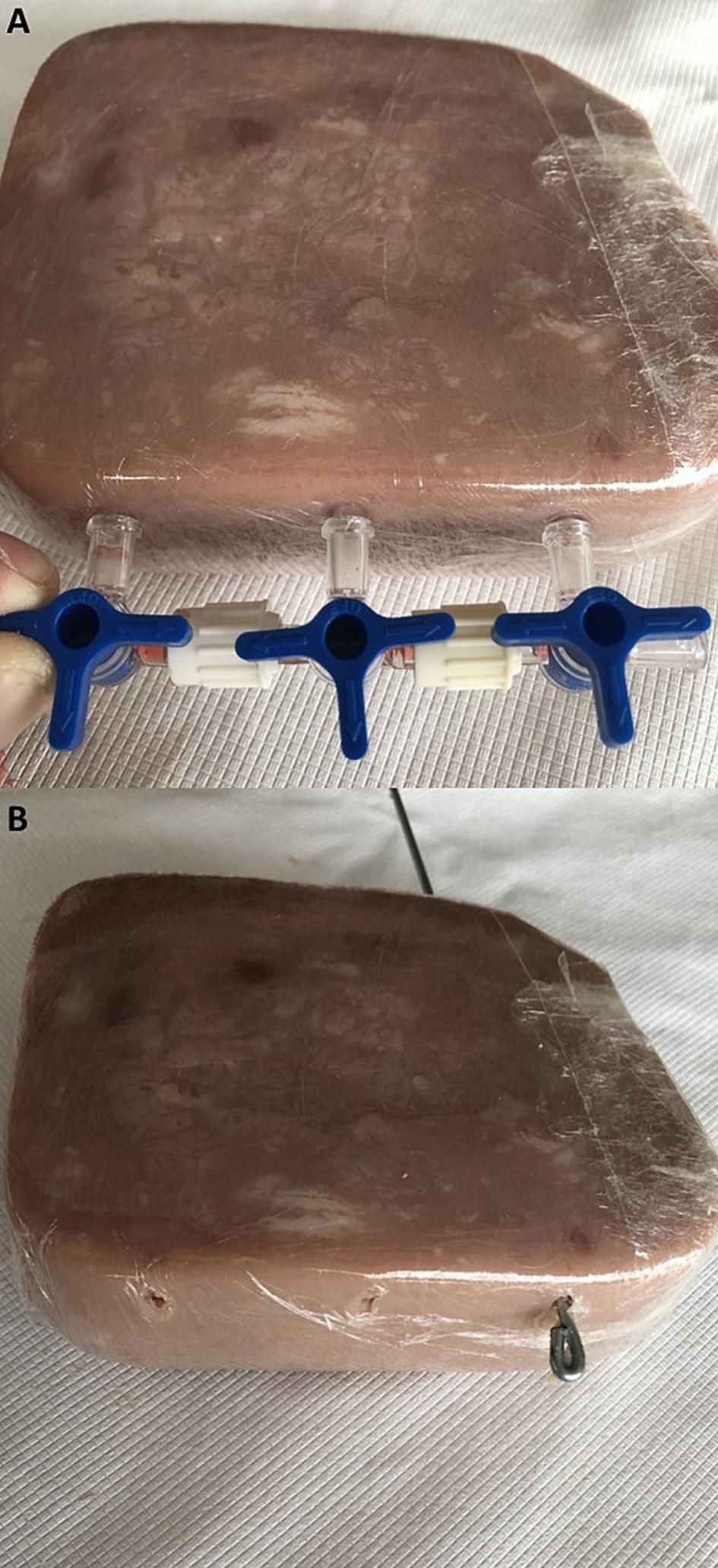
MethodologyBegin the construction of the model by connecting an IV-line infusion kit to a saline solution bag, connect a 3-way stopcock at the end of the line and in the two remaining ports of the 3-way stopcock, attach a 20 ml syringe and an IV extension. Continue by covering the piece of pork ham with the plastic wrap and connect the remaining 3-way stopcocks with each other.
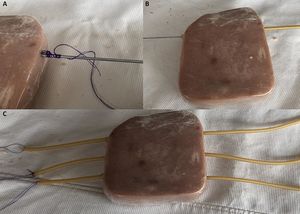
To place the rubber tubes inside the pork ham cube, mark three dots at one of the sides of the ham making small ruptures in the plastic wrap. Use the ports of the 3-way stopcocks assembled previously as a reference for making the marks (Fig. 2-A). Mark the ham 5 mm beneath the upper ham’s surface.
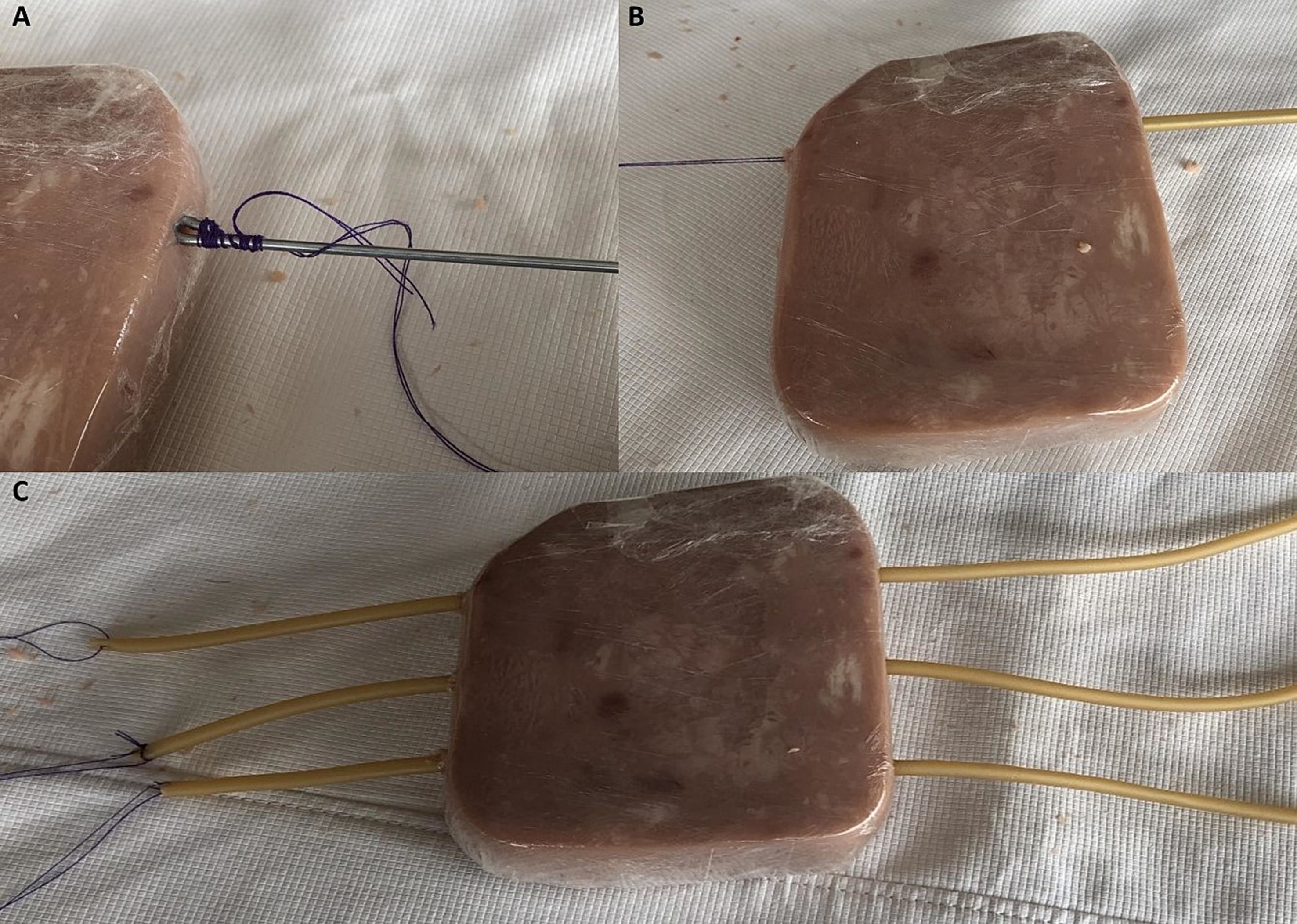
Insert the aluminum wire into the ham through the marks and following the longitudinal axis of the piece, perforate it in a straight and parallel manner. Flexing the tip of the wire and pulling it in and out several times will create a tunnel in the ham in which the rubber tube will be embedded in the next step (Fig. 2-B).
Make three to four stiches to one of the extremes of each rubber tube, tie the thread to the extreme of the wire with the flexed tip (Fig. 3-A). Pass the wire with the tied thread through one of the tunnels and extract the wire. (Fig. 3-B). Pull the thread and insert the rubber tube into the ham (Fig. 3-C).
Attach the rubber tubes to the three 3-way-stopcocks previously assembled, a plastic belt can be wrapped around the rubber tube and the 3-way stopcock to which it is attached to avoid leaks. Bring the 3-way stopcocks closer to the ham by pulling the three rubber tubes. Let saline solution flow through the whole system and through the rubber tubes. Tie three knots in the free end of the plastic tubes to close the system. The final product should look like the model portrayed in fig. 4.
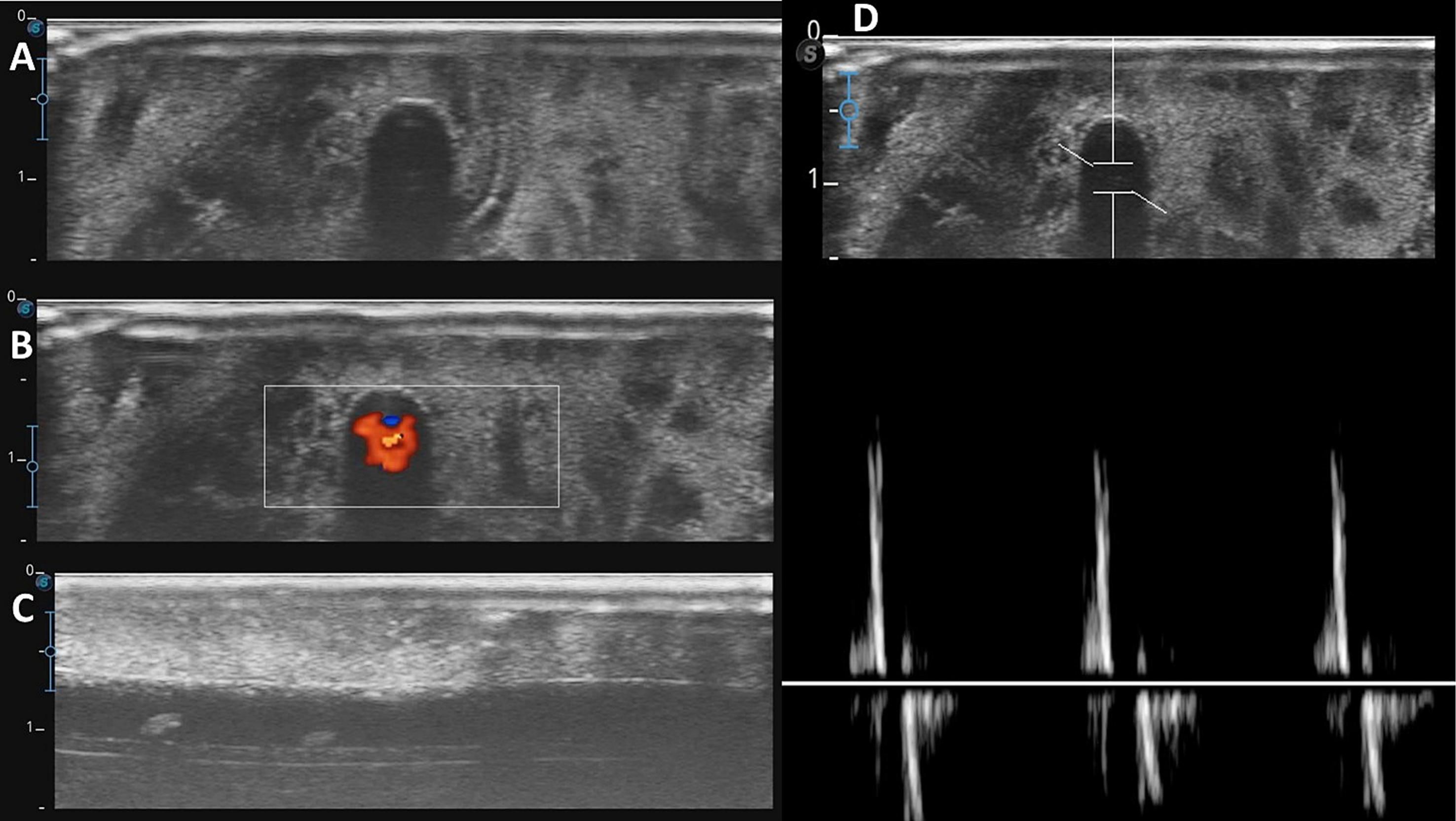
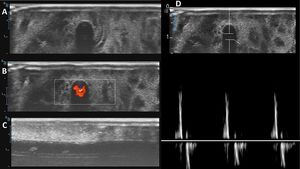
ResultsThis 3-vessel model can be used for practicing palpation or ultrasound-guided artery cannulation techniques, since pulsatile pressure can be applied to the target vessel using the 20 ml syringe attached to the irrigation system. Depending on the distance from the ham’s surface to the rubber tube, the pulsatile pressure can be felt. The mean reported distance from the skin to the anterior wall of the radial artery is 1.99 ± 0.99 mm,10 considering the 2.5 mm diameter rubber tubes and making the center of the tunnel 5 mm beneath the ham’s surface should provide a distance between the ham’s surface and the anterior wall of the rubber tube of 2.5 mm approximately, making the pulsatile rubber tube palpable.
“In-plane” and “out-of-plane”ultrasound-guided techniques can be practiced. Our model provides images that resemble an arterial vessel, if a constant and pulsatile pressure is applied to the system with the syringe, when examined with color doppler and pulsated wave doppler on ultrasound, the images will show a pulsated flow (Fig. 5). After puncturing the target vessel in the model, a pulsatile flow can be observed out through the cannulation system used in the practice.
The same vessel can be punctured more than 10 times before observing leaks through the ham’s tissue. This allow the model to be stored and used by 3 different groups in different sessions. Both Seldinger and modified Seldinger techniques can be practiced with this model. Cleaning with air or solution the cannula’s lumen after puncturing the ham may improve the flow through the cannula since it can become clogged with ham after several punctures.
This model has been used in our institution by cardiology fellows for practice. Self-confidence for preforming the procedure before and after practicing with our model was questioned and graded in a scale from 1 to 10, 1 being no confidence and 10 being the highest level of confidence. 32 residents had a 1-hour practice with our model. Before practicing, 28% reported a level of self-confidence of 10 and 9% a self-confidence of 9. After practicing, 50% reported a level of self-confidence of 10 and 22% a self-confidence of 9.
ConclusionSince its beginning, medicine has relied on invasive procedures to treat patients. These procedures are constantly evolving and every day, better techniques are described, and better tools are designed to achieve better and safer results. Practice and repetition are fundamental steps in the process of learning, and nowadays practicing models are commonly used by medical residents, fellows, and students to achieve a successful and safe procedure in a real situation.
Other practicing models have proved to be useful in improving the success rate of ultrasound-guided radial artery cannulation in the first attempt.9 We present a low-cost practicing model for radial artery cannulation that can be built rapidly, with simple materials, and that can be adopted by Hospitals with scarce resources to teach and master radial artery cannulation. We believe that this practicing model will improve radial artery cannulation success rate in the first attempt by residents in teaching Hospitals that adopt its use to their training program. A prospective study could validate our model as teaching tool in the process of achieving a successful radial artery cannulation.
Declaration of interestsNone of the authors have a conflict to declare.
Ethics comittee aprovalDue to the characteristics of the study, it did not have to be approved by the ethics committee of the institution in which we work. The present work is a report of a training model in which no patient’s data were obtained, disclosed, or documented. As well as no diagnostic or therapeutic intervention was made in a patient or animal during the report.
Informed consent of participantsDue to the characteristics of the study, there was no participation of patients. No informed consent had to be singed or printed.
FundingThe funding of this work was provided by the authors own goods. No third parties were involved in the funding of this project.