The evolution of empathy among medical students according to gender and specialty preference is explored using several validated scales. The value of our feedback to the medical students at the end of the study is also assessed.
Materials and methodsA total of 151 students completed the initial questionnaire, including the following scales: Jefferson Scale of Physician Empathy (JSPE), Interpersonal Reactivity Index (IRI), and Empathy Quotient (EQ). The final questionnaire was completed by 99 of them.
ResultsAccording to the EQ classification, it was found that 7.3% of students had low empathy, 49.7% average, 36.4% above average, and 6.6% very high. Empathy was higher among women in IRI-FS, IRI-EC, and EQ. Students who preferred people-oriented specialties score higher in JSPE and EQ. The IRI-Fantasy Scale was the only scale that shows increased scores on follow-up and in students with preference for people-oriented specialties.
DiscussionThis study shows that most of the medical students in our sample had a good level of empathy. Empathy was unchanged throughout the follow-up. Medical students had different profiles of empathy. In extreme profiles, feedback could offer advice in the process of choosing a specialty to best suit their empathic skills.
Se explora la evolución de la empatía en estudiantes de medicina utilizando a la vez varias escalas validadas, teniendo en cuenta el sexo y la preferencia de especialidad. Al final del estudio se realizó feedback de los resultados a los estudiantes.
Materiales y métodosCiento cincuenta y un estudiantes de medicina completaron el cuestionario inicial con las siguientes escalas: Jefferson Scale of Physician Empathy, Interpersonal Reactivity Index (IRI), Empathy Quotient (EQ) y Systemizing Quotient. Noventa y nueve de ellos finalizaron el estudio de seguimiento.
ResultadosSegún la clasificación de la EQ encontramos un 7,3% de estudiantes con baja empatía, un 49,7% media, un 36,4% por encima de la media y un 6,6% muy alta. La empatía fue mayor en mujeres en IRI-Fantasy Scale, IRI-Empathetic Concern y EQ. En los estudiantes con preferencia de especialidad orientada a las personas la empatía fue mayor en Jefferson Scale of Physician Empathy y EQ. IRI-Fantasy Scale fue la única escala que aumentó durante el seguimiento y en los estudiantes con orientación a las personas.
DiscusiónEste estudio mostró que la mayoría de los estudiantes de medicina de nuestra muestra tenían un buen nivel de empatía, y que la empatía apenas se modificó durante el período de seguimiento. Los estudiantes de medicina tenían diferentes perfiles de empatía, algunos de ellos con valores extremos. En estos perfiles el feedback permite ofrecer asesoramiento en el proceso de elegir una especialidad para adaptarse mejor a sus habilidades empáticas.
Empathy is the ability to identify and understand the thoughts and feelings of others and to respond with appropriate emotions.1 Medical empathy has been defined as the predominantly cognitive attribute that involves the ability to understand patient's experiences, concerns, and perspectives, and communicate this understanding with the intention of helping.2,3 All else being equal, a doctor who understands a patient's thoughts and feelings can provide better care.4 The two most commonly used instruments in empathy research and Medical Education setting are the JSPE (Jefferson Scale of Physician Empathy) and the IRI (Interpersonal Reactivity Index). JSPE measures empathy specifically in medical students and physicians in the context of patient care, and considers empathy as a predominantly cognitive attribute. IRI is a multidimensional approach that permits discrimination between cognitive [IRI-PT (IRI-Perspective-Taking) and IRI-FS (IRI-Fantasy Scale)] and affective empathy [IRI-Empathetic Concern (IRI-EC) and IRI-PD (IRI-Personal Distress)].5,6 EQ (Empathy Quotient) and SQ (Systemizing Quotient) questionnaires are less used but can complement the study of empathy as it relates to specialty preference. EQ and SQ allows the categorization of scores in four groups: low, average, above average and very high, facilitating comparison between groups. EQ and SQ are based on a psychological model with two dimensions, empathy and systematizing, and were proposed by Baron-Cohen. Systematizing is defined as the aptitude to analyze and build systems based on procedure. Research shows that men systematize better than women and women have more empathy than men.7 Colleges students in which systematizing prevail tend to choose technological careers regardless of their gender.8
To date, studies using the JSPE2,6,9–19 and IRI scales6 show mixed results in correlating levels of empathy in medical students with gender. Similarly, some studies on specialty preference show higher empathy scores in students with people-oriented versus technology-oriented specialties2,9–12,14,17,20 while others do not find a significant difference.12,15,18,21
Most of the studies suggest that empathy diminishes after the third year of medical school.9,10,20,22–26 However, recent studies27,28 dispute this statement, since most of the longitudinal studies do not show changes in the empathy scores over time.
The aim of this research is to address these uncertainties with a longitudinal study that explore the evolution of empathy in medical students using several scales simultaneously (JSPE, IRI, EQ and SQ) and stratified evolution according to gender and specialty preference. At the end of the study, we provided individual feedback of the results to all participating students. That allowed them to know their empathy level and made them aware of the important role that empathy plays in choosing their specialty.
Materials and methodsStudy population consisted of medical students from the Faculty of Medicine, University of Lleida (UdL) in Spain. The sample was 151 students who volunteered with informed consent to participate in this study. Ninety-nine students completed the follow-up study, giving a dropout rate 34.4%. The period of follow-up was two years in 21.21% and one year in 78.79% of medical students.
All medical students completed the initial questionnaire online with the following self-administered measurement instruments:
1. JSPE consists of 20 items with score ranges between 20 and 140. It measures empathy in the context of medical education and patient care.2 JSPE has been used in most of the studies done with medical students. It has been translated from English to Spanish and validated in Spanish.4
2. IRI consists of 4 subscales of 7 items each with scores ranging from 0 to 28. Two subscales measure cognitive empathy (IRI-PT and IRI-FS) and two subscales measure affective empathy (IRI-EC and IRI-PD).5,29
3. EQ consists of 60 items, 40 measure empathy and 20 measure control. Scores range from 0 to 80. It measures cognitive and affective empathy in adults. EQ also allows the classification of empathy level into the four categories of low, average, above average and very high. The version used, which has not been validated in Spanish, was obtained from http://espectroautista.info/tests/espectro-autista/adultos/EQ. We have author's consent for EQ questionnaire.1
4. SQ consists of 60 items, 40 measure systematization and 20 measure control. Scores range from 0 to 80. It measures the ability for systematizing in adults. SQ allows the classification of systemizing into the four categories of low, average, above average and very high. The version used, which has not been validated in Spanish, was obtained from http://espectroautista.info/tests/espectro-autista/adultos/SQ. We have author's consent for SQ questionnaire.7
5. Specialty preference classification is based on Hojat's study2,9 which defines two categories of professional preference: 1. People-oriented specialties. 2. Technology-oriented specialties.
The questionnaire administered at the end of the study used the same measurement scales as the initial test.
Feedback. To ensure confidentiality, only the principal investigator, a clinical psychiatrist, had access to the results and reported results individually to all the participating students (N=151). We offered students the option of receiving their individual results during a face to face meeting or by email. The students who chose the return by email were sent the report of the results to the email address they authorized themselves. The individual report contained the following: an introduction to empathy, criteria used for result's interpretation and guidelines to improve empathic skills. The students who chose a face to face option were given an appointment with the psychiatrist research, the report results was given to them individually, the report were explained and any doubts expressed by the student regarding their abilities were solved, as well as the difficulties they presented in the relationship with the patient. The in-person meeting allowed individual feedback between the medical students and principal investigator and provided qualitative information based on their reflections during the semi-structured interview. To evaluate study utility and satisfaction, a survey is given. The survey consists of four questions with a Yes/No closed answer: 1. Has this study increased your self-knowledge? 2. Do you think that you will bear empathy in mind in your professional future as a doctor? 3. Do you think this study may help medical students to choose a specialty according to their personal skills? 4. Do you think it would be useful to implement workshops during medical school to maintain and improve empathy?
The scores of the empathy scales were described with medians and interquartile ranges (IQR) as they showed a non-normal distribution, assessed by means of the Shapiro–Wilk test. Differences in basal empathy levels in the whole study population by sex and specialty preference were analyzed with the Mann–Whitney U test. To assess the evolution of the empathy we performed paired Mann–Whitney U test. All tests were bilateral, setting the significance level to 0.05. All analyses were carried out with the statistical package R.
This project was approved by the Ethics Committee for Clinical Research of Lleida CEIC-1515.
ResultsThe median (IQR) age was 22 (21–23) years old, 78.8% of the students were women and 67.5% expressed preference for people-oriented specialties. According to EQ classification we found 7.3% of students with low empathy, 49.7% average, 36.4% above average and 6.6% very high.
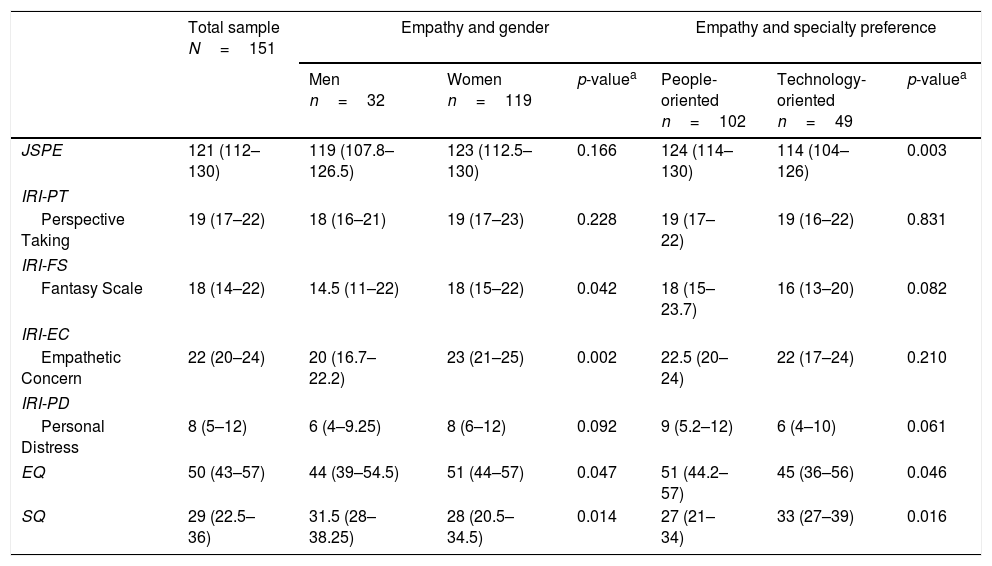
Empathy was significantly higher in women in subscales IRI-FS, IRI-EC and EQ. We found statistically significant differences in SQ between genders, being higher in men. There were no statistically significant gender differences in the JSPE. Regarding specialty preference, medical students with a higher score in JSPE and EQ preferred people-oriented specialties. Students with a preference for technology-oriented specialties had a higher score in SQ. The relationship between empathy measured by IRI and specialty preference did not show statistically significant differences (Table 1).
Descriptive and bivariate analysis of different scales of empathy stratified according to gender and specialty preference.
| Total sample N=151 | Empathy and gender | Empathy and specialty preference | |||||
|---|---|---|---|---|---|---|---|
| Men n=32 | Women n=119 | p-valuea | People-oriented n=102 | Technology-oriented n=49 | p-valuea | ||
| JSPE | 121 (112–130) | 119 (107.8–126.5) | 123 (112.5–130) | 0.166 | 124 (114–130) | 114 (104–126) | 0.003 |
| IRI-PT | |||||||
| Perspective Taking | 19 (17–22) | 18 (16–21) | 19 (17–23) | 0.228 | 19 (17–22) | 19 (16–22) | 0.831 |
| IRI-FS | |||||||
| Fantasy Scale | 18 (14–22) | 14.5 (11–22) | 18 (15–22) | 0.042 | 18 (15–23.7) | 16 (13–20) | 0.082 |
| IRI-EC | |||||||
| Empathetic Concern | 22 (20–24) | 20 (16.7–22.2) | 23 (21–25) | 0.002 | 22.5 (20–24) | 22 (17–24) | 0.210 |
| IRI-PD | |||||||
| Personal Distress | 8 (5–12) | 6 (4–9.25) | 8 (6–12) | 0.092 | 9 (5.2–12) | 6 (4–10) | 0.061 |
| EQ | 50 (43–57) | 44 (39–54.5) | 51 (44–57) | 0.047 | 51 (44.2–57) | 45 (36–56) | 0.046 |
| SQ | 29 (22.5–36) | 31.5 (28–38.25) | 28 (20.5–34.5) | 0.014 | 27 (21–34) | 33 (27–39) | 0.016 |
Variables are described with medians and interquartile ranges.
JSPE: Jefferson Scale of Physician Empathy; IRI: Interpersonal Reactivity Index; EQ: Empathy Quotient; SQ: Systemizing Quotient.
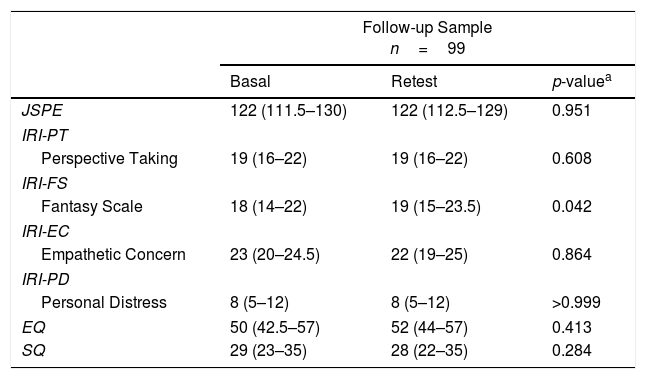
Table 2 shows the evolution of scales of empathy in the follow-up sample (n=99), which will be valid sample of analysis. We found statistically significant differences in the subscale IRI-FS, with higher scores in the retest.
Evolution of empathy in follow-up sample between the test and retest in different scales of empathy.
| Follow-up Sample n=99 | |||
|---|---|---|---|
| Basal | Retest | p-valuea | |
| JSPE | 122 (111.5–130) | 122 (112.5–129) | 0.951 |
| IRI-PT | |||
| Perspective Taking | 19 (16–22) | 19 (16–22) | 0.608 |
| IRI-FS | |||
| Fantasy Scale | 18 (14–22) | 19 (15–23.5) | 0.042 |
| IRI-EC | |||
| Empathetic Concern | 23 (20–24.5) | 22 (19–25) | 0.864 |
| IRI-PD | |||
| Personal Distress | 8 (5–12) | 8 (5–12) | >0.999 |
| EQ | 50 (42.5–57) | 52 (44–57) | 0.413 |
| SQ | 29 (23–35) | 28 (22–35) | 0.284 |
Variables are described with medians and interquartile ranges.
JSPE: Jefferson Scale of Physician Empathy; IRI: Interpersonal Reactivity Index; EQ: Empathy Quotient; SQ: Systemizing Quotient.
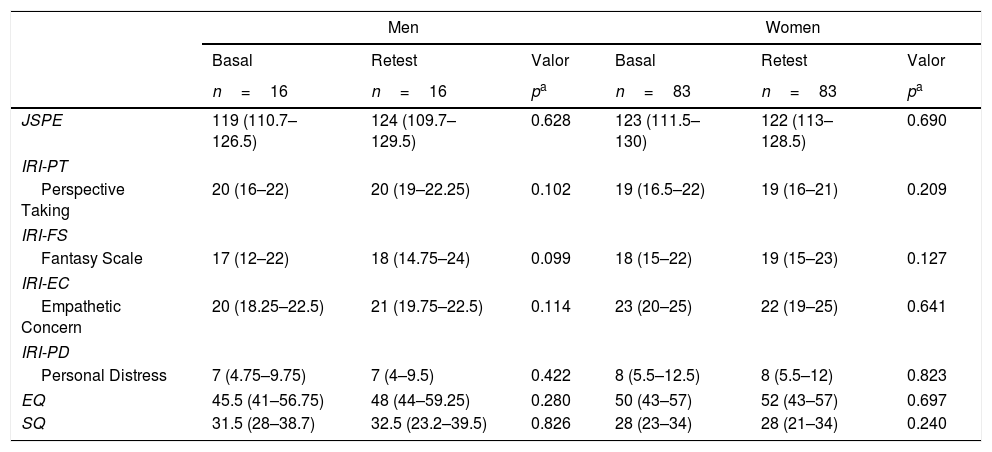
Table 3 shows the evolution of empathy stratified according to gender and specialty preference. Although women had higher basal fantasy score and increase in retest, no differences were found between the test and the retest according to gender. We found statistically significant trend in subscale IRI-FS in medical students with people-oriented specialties, in which we observed an increase in the retest. This difference was not observed among students that prefer technology-oriented specialties.
Evolution of empathy between the test and retest in different scales of empathy stratified according to gender and to specialty preference.
| Men | Women | |||||
|---|---|---|---|---|---|---|
| Basal | Retest | Valor | Basal | Retest | Valor | |
| n=16 | n=16 | pa | n=83 | n=83 | pa | |
| JSPE | 119 (110.7–126.5) | 124 (109.7–129.5) | 0.628 | 123 (111.5–130) | 122 (113–128.5) | 0.690 |
| IRI-PT | ||||||
| Perspective Taking | 20 (16–22) | 20 (19–22.25) | 0.102 | 19 (16.5–22) | 19 (16–21) | 0.209 |
| IRI-FS | ||||||
| Fantasy Scale | 17 (12–22) | 18 (14.75–24) | 0.099 | 18 (15–22) | 19 (15–23) | 0.127 |
| IRI-EC | ||||||
| Empathetic Concern | 20 (18.25–22.5) | 21 (19.75–22.5) | 0.114 | 23 (20–25) | 22 (19–25) | 0.641 |
| IRI-PD | ||||||
| Personal Distress | 7 (4.75–9.75) | 7 (4–9.5) | 0.422 | 8 (5.5–12.5) | 8 (5.5–12) | 0.823 |
| EQ | 45.5 (41–56.75) | 48 (44–59.25) | 0.280 | 50 (43–57) | 52 (43–57) | 0.697 |
| SQ | 31.5 (28–38.7) | 32.5 (23.2–39.5) | 0.826 | 28 (23–34) | 28 (21–34) | 0.240 |
| People-oriented specialties | Technology-oriented specialties | |||||
|---|---|---|---|---|---|---|
| Basal | Retest | Valor | Basal | Retest | Valor | |
| n=68 | n=68 | pa | n=31 | n=31 | pa | |
| JSPE | 125 (114–130) | 124 (114–129) | 0.554 | 114 (103–128) | 120 (108.5–127.5) | 0.449 |
| IRI-PT | ||||||
| Perspective Taking | 19 (16.75–22) | 19.5 (16–22) | 0.427 | 19 (16–20.5) | 19 (16–21) | 0.982 |
| IRI-FS | ||||||
| Fantasy Scale | 18 (15.75–24) | 20 (15–24) | 0.0503 | 16 (12.5–20) | 16 (14–19.5) | 0.448 |
| IRI-EC | ||||||
| Empathetic Concern | 23 (20–25) | 22 (20–25) | 0.824 | 23 (18–24) | 22 (17.5–24.5) | 0.990 |
| IRI-PD | ||||||
| Personal Distress | 9 (6–13) | 9 (6–12) | 0.932 | 6 (3.5–8.5) | 7 (4.5–10.5) | 0.836 |
| EQ | 51 (43.75–57.25) | 52.5 (44–58) | 0.389 | 45 (38–57) | 47 (37.5–56.5) | 0.929 |
| SQ | 27 (23–34) | 27 (21–35) | 0.589 | 33 (27–36) | 31 (25–40) | 0.284 |
Variables are described with medians and interquartile ranges.
JSPE: Jefferson Scale of Physician Empathy; IRI: Interpersonal Reactivity Index; EQ: Empathy Quotient; SQ: Systemizing Quotient.
Feedback. A report with the results was delivered to 151 participating students. In 77.8% of cases it was sent by email, while 22.2% of the students came for an individual interview and completed satisfaction survey. Results of the survey showed that 85.7% of the students thought the study increased their self-knowledge, 100% affirmed that they will bear empathy in mind in their professional future as a doctor, 85.7% thought that this study can help medical students to choose a specialty according to their personal skills, and 100% agreed that it would be useful to implement workshops during medical school to help maintain and improve empathy.
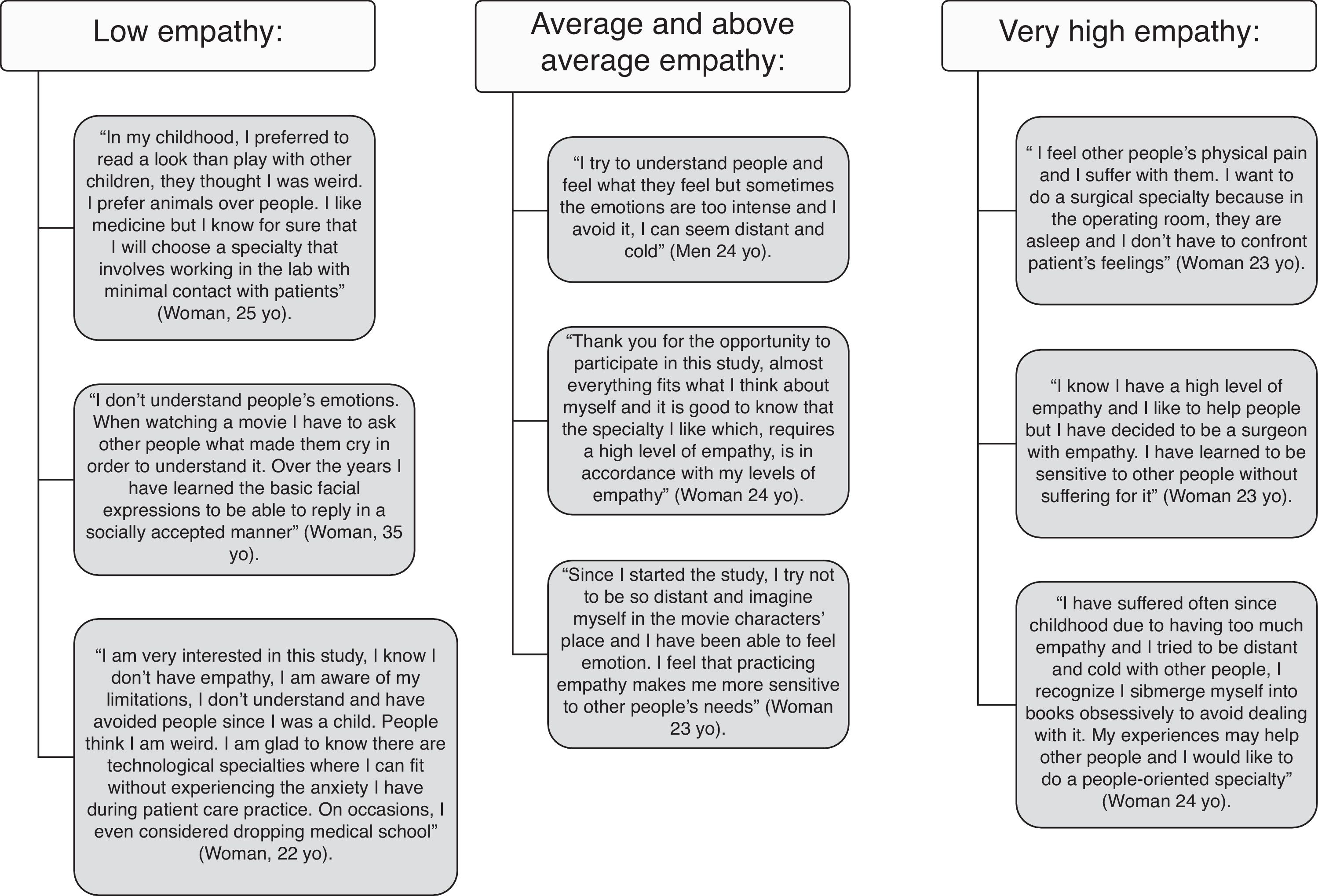
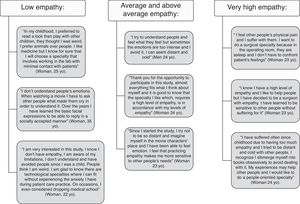
It is important to mention that feedback was more useful for medical students with extreme scores of empathy on EQ categories. Low empathy means EQ scores in the range 0–32 (for comparison, the average for individuals with Autistic Spectrum Disorders is 20)1 and very high empathy means EQ scores in the range 64–80. The interview conducted by a psychiatrist allowed symptoms detection of pathological grief, adaptive disorders, social anxiety disorders (in high extreme scores of empathy), and in some case, autistic spectrum traits (in extremely low scores of empathy). In these cases, students appreciated having a space that allowed them to express the discomfort they feel and that interferes both in their academic outcomes and in their social adaptation. The semi-structured interview allowed medical students to recognize their personal difficulties and accepted help in choosing a specialty. In some cases professional help was recommended. Fig. 1 shows some of the reflections of the medical students during the feedback.
DiscussionOur research explored the evolution of empathy in medical students using several scales simultaneously and stratified evolution according to gender and specialty preference.
Compared to previous studies, in our sample we observed higher scores of empathy in JSPE,11,13,15,22,24–26,30,31 in EQ,32 and in subscales IRI-FS5,33 and IRI-EC.16,32,33 In IRI-PT we found higher scores compared to some studies5,33,34 and similar scores to others.16,28,32 In the subscale IRI-PD our scores were lower.5,28 These differences could be explained by intercultural variability among different countries.35
We have not found in the literature other studies that use these three empathy scales (JSPE, EQ and IRI). Although depending on the empathy scale used the researchers might get very different results, in our study the use of different scales based on different theoretical models has allowed us to reach these results. It has also allowed us to observe differences in gender. Empathy is higher in women in EQ, IRI-FS, and IRI-EC but there are no gender differences in JSPE.6,12 We find that the systemizing ability measured by SQ is higher in males, as was suggested by the SQ authors.7
When we analyzed the relationship between empathy and specialty preference in medical students, we found higher scores in JSPE and EQ in students with people-oriented specialties, consistent with previous studies.2,9,12,14,17,20 Medical students with technology-oriented specialties have low empathy scores and systemizing ability measured by SQ prevails. The differences in scale scores we found between men and women provide an explanation for the higher percentage of technology-oriented specialty preference in males, as seen in the model presented by Baron-Cohen.8
As other recent longitudinal studies showed,27,28 empathy scores in JSPE and EQ did not change in our study and, in general, medical students maintained empathy scores. IRI-FS is the only empathy scale that increased in the retest. This subscale reflects the student's ability to imagine themselves in the perspective of characters in art, literature, cinema, and video games. Although women had higher scores in basal fantasy and they increased in the retest, differences were not statistically significant. We also wish to emphasize that in medical students with people-oriented specialties, fantasy was higher and increased in the retest.
Despite the finding that subscale IRI-PD was higher in women and in students with people-oriented specialties, the differences were not statistically significant. Nevertheless, is the only scale that permits the identification of medical students with high anxiety levels in interpersonal relationships. To develop and keep empathy alive, it is necessary to avoid over-concern with oneself.36 Some authors considered subscales IRI-PT and IRI-EC relevant for patient care.16,37,38 We think that neither IRI-FS nor IRI-PD can be dismissed, since they provide relevant information as to how the student approaches the doctor–patient relationship, and when coupled with SQ, help to guide specialty preference in medical students.
Qualitatively, the interview of results report done in our study, offers the student the opportunity to discuss difficulties with patient interactions and to resolve doubts regarding specialty preference. If such interviews are to be undertaken, we emphasize the need to allocate the time and trained professionals for it.
Previous longitudinal studies reviewed did not show a decrease in empathy.11,16,30,31 Indeed, deliberately promoting an empathic attitude could favor people-oriented specialties at the expense of technological-oriented ones.11 Therefore, the main socio-scientific interest of this study would be, not to increase empathic ability but to offer guidance to medical students in the process of choosing a specialty depending on their skills, including empathy. Most of the medical students in this study showed a reasonable score in both, empathy and systemizing ability, being able to pursue either a medical or a surgical specialty.
We would like to highlight the individualized feedback, which adds value and directly benefits the medical students and we are expecting some sort of long-term patient care benefit. All participants received their own empathy results and guidelines for improving empathic ability. Both those who interviewed and those who received the report by email, are offered the possibility to resolve any questions that arise when choosing the specialty. Guidance in choosing a specialty is most important for students with low levels of empathy, students who may have had difficulties in social relationships since childhood and feel anxiety in front of a patient. Similarly, medical students with very high empathy scores must be cautious in choosing a specialty, as shown in their reflections in Figure 1. These students with extreme scores justify the design of future qualitative studies. Although almost all medical training emphasises that medicine includes many different specialties based on different cognitive and emotional resources, and not all of them require high levels of empathy, we think it is essential for the medical student to be aware of it, before choosing the specialty. This awareness will allow students to best find the vocation most suited to their talents, accomplishing the primary goal of medicine, helping patients.
This issue of matching empathic measures to medical specialties opens multiple lines of longitudinal research to help obtain effective measures to better guide students during medical school and to verify whether the above-mentioned measures are useful in guiding their professional career. Also, tracking student perceptions and views in clinical teaching, can be very helpful in better developing and refining a preclinical curriculum, assessing its the strengths and shortcomings.
In future work we must also take into account other factors that are yet insufficiently understood which may influence the development of empathy and professional guidance, such as cultural characteristics of the population, including cultural background, undergraduate curricula and positive role models.
When planning strategies to improve communication with the patient and skills regarding empathy, we feel that psycho-educational interventions should be focused on promoting perspective taking. With this in mind, our team carried out an experimental workshop of sensory deprivation in which medical students learn to identify emotions that they experience when pretending to be a person with various disabilities, and we observed an increase in JSPE scores.39 Other strategies that we consider important in the medical student's education would be the re-education of inadequate emotional response, development of personal experiences, and diminishing personal distress that generates from the doctor–patient relationship. In these cases it would be interesting to offer a space in which he can express the discomfort he feels and, if necessary, professional help. We must therefore help medical students recognize their virtues and weaknesses, helping them to best find their place within the medical profession and society.
Limitations. In our observational study, medical students were invited to participate voluntarily and it was not possible to calculate the sample size previously.
Although JSPE and IRI have been validated and widely used in the empathy research, the other two scales, EQ and SQ, require further validation, as they may measure different constructs. However, EQ is the only one that allows the classification of empathy in four groups facilitating the comparison between different samples.
The low proportion of males was a limitation of our study, and reflected the increased proportion of women attending medical school, more than 70% in Spain.40
The high dropout rate (34.4%) might affect the interpretation of the results. The small number of longitudinal studies, and the generally small number of samples per center, reflected the difficulties of carrying out such studies on medical students.16,41,42 These difficulties included a lack of participation by medical students in research studies and a tendency to drop out before the end. According to the students themselves, this reflected a lack of time after prioritizing their curricular activities and a lack of interest. This lack of participation in research studies was consistent with a lower level of attendance to elective classes.43 Furthermore, the personal interviews with students suggested that anxiety regarding the results is another possibility. All the students who participated in the study were given a report with the results, though, not all of them agreed to go in depth the same way. Since this proposed initiative as well as the workshops were well received, we are encouraged to continue in this way.
In summary, our study shows that most of the medical students in our sample had a good level of empathy and empathy was unchanged throughout the follow-up. Medical students had different profiles of empathy, some falling in extremes of high and low empathy. In these profiles, feedback could offer advice in the process of choosing a specialty to best suit their empathic skills.
Conflict of interestThe authors of this article declare no conflict of interest.
The authors are deeply grateful for collaboration from medical students of University of Lleida. We thank the Biostatistics Unit of the IRBLleida, especially Carles Forné for their helpful statistical advices. We sincerely thank Dr. Elena Cucurull and Dr. David Norwood for their helpful review of the manuscript. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.