The authors aimed to compare two different empathy scales across the six-year medical course, among undergraduate medical students attending a school of medicine that was established nine years ago in the Brazilian city of São Paulo.
MethodCross-sectional study. The authors evaluated a sample of 296 students. The empathy evaluation was performed using the Jefferson Scale of Physician Empathy (JSPE), version for medical students, and Davis's multidimensional Interpersonal Reactivity Index (IRI-Brazilian version), applying both to each student simultaneously. The students were divided into three groups, according to their year on the medical course: Basic Group (1st and 2nd years), Clinical Group (3rd and 4th years) and Clerkship Group (5th and 6th years). Socio-demographic data and empathy scores, for both scales, were compared between these three groups using the Chi-square test and the Kruskal–Wallis test, as applicable.
Resultsthe JSPE scores were similar among the students from the Basic, Clinical and Clerkship groups (p=0.53). On the other hand, the affective dimension of IRI-Brazilian version revealed a significantly lower score in the Clerkship Group (p<0.01).
ConclusionsThe authors suggest that the level of empathy can change, and in this case, the affective dimension was most affected during medical school.
El objetivo de los autores fue comparar dos escalas diferentes de empatía a lo largo de la carrera de medicina de seis años, entre los estudiantes que asistían a una escuela de medicina fundada nueve años atrás en la ciudad brasileña de São Paulo.
MétodoEstudio transversal. Los autores evaluaron una muestra de 296 estudiantes. La evaluación de la empatía se realizó utilizando la Escala de Empatía de los Médicos de Jefferson (JSPE), versión para estudiantes de medicina, y el Índice de Reactividad Interpersonal multidimensional de Davis (IRI-versión brasileña), aplicando ambos de manera simultánea a cada estudiante. Se dividió a los estudiantes en tres grupos, con arreglo a su curso de carrera de medicina: Grupo básico (1er y 2° años), Grupo Clínico (3r° y 4° años) y Grupo de Prácticas (5° y 6° años). Se compararon los datos socio-demográficos y las puntuaciones sobre empatía entre estos tres grupos, utilizando las pruebas χ2 y Kruskal-Wallis, según el caso.
ResultadosLas puntuaciones JSPE fueron similares entre los estudiantes de los grupos básico, clínico y de prácticas (p=0,53). Por otro lado, la dimensión afectiva de la versión brasileña de IRI reveló una puntuación inferior en el Grupo de Prácticas (p<0,01).
ConclusionesLos autores sugieren que el nivel de empatía puede cambiar y que, en este caso, la dimensión afectiva se vio más afectada durante la enseñanza de medicina.
Some studies suggest that a drastic change takes place in the medical student during their training process. In the early years of medical training, most students are thrilled with the idea of becoming a physician, and are more sensitive to patients’ suffering.1,2 During the medical course, this idealism can decrease, along with a process of “dehumanization”,3 in which the patient takes a secondary role in the medical practice.
One point that is acknowledged is that the medical student is exposed to a huge amount of scientific information that monopolizes their educational time,4 and rarely leaves room to address issues relating to the understanding of patients’ expectations.5 To provide quality care, skills are needed to help the doctor not only to know about the disease, but also to understand the human being who is sick. Among these skills, empathy has proven to be crucial.6 Studies show that empathy among physicians is associated with better patient satisfaction,7,8 better adherence to treatment,8,9 more favorable clinical outcomes,10–13 and a decrease in the number of malpractice claims.14
The word empathy originates from the Greek word empatheia, meaning appreciation of the feelings of another person. The English term empathy was introduced by the psychologist Edward Titchener Bradner, and is used to mean the ability to understand another human being. Years later, Elmer Ernest Southard used the concept of empathy in the context of the doctor and patient, as a facilitator of diagnosis and therapy.15
There is disagreement among psychoanalysis scholars regarding the attributes involved in empathy. Some authors consider empathy to be a predominantly cognitive attribute,16,17 linking it to an understanding of the patient's experiences and concerns, combined with the ability to communicate.18 Other authors see empathy essentially as belonging to the affective dimension, determined by the ability to experience the feelings of the other person.19 In this case, it is a consequence of the ability to be empathic, and it implies a spontaneous feeling of identification with the sufferer, in a process that involves emotion.
Some tools have recently been described to measure empathy. These include: the Interpersonal Reactivity Index (IRI) developed by Davis20 with a version validated and adapted for Brazil (Escala Multidimensional de Reatividade Interperssonal – EMRI),21 the Hogan Empathy Scale22 and the Measure of Emotional Empathy developed by Mehrabian and Epstein.23 The Jefferson Scale of Physician Empathy (JSPE) was specifically created for the patient care and medical education context.24 Authors who have used some of these instruments have shown that during the training of different health professionals, empathy can provide positive or negative changes.6
A cross-sectional study by Chen et al.,25 identified a low empathy score (measured through the JSPE scale) among 3rd year medical school students, compared to 2nd year students. A cohort study by Hojat et al.,6 identified an erosion of empathy (using JSPE as a tool to assess empathy) occurring in medical school, with the lowest scores among 3rd year students.
Understanding and assessing the degree of empathy of medical students during medical school is an important issue to be addressed during medical training. The aim of this study was to evaluate the degree of empathy among medical students in different years of the course at the Private University of São Paulo, using two different instruments: the JSPE (to assess the principally cognitive dimension of empathy for specific medical students within the medical context) and the IRI-Brazilian version (to assess the cognitive and affective dimension for the population in general, not specific to the medical context).
MethodologyStudy designWe included medical students from a private University in the in the city of São Paulo, which was established nine year ago. The total number of medical students in that University was 577. The students were invited to take part during the curricular classes. Adherence to the study was voluntary, and was related to the presence of the student in the classroom when the survey was administered. The data collection was carried out from September to December 2013. All the participants signed an informed consent form, and the study protocol was approved by the local ethics committee and by the ethics committee of the University of São Paulo School of Medicine.
InstrumentsTwo tools were used to evaluate the students’ empathy: the Jefferson Scale of Physician Empathy (JSPE) and the IRI-Brazilian version. These were applied simultaneously to each participating student.
The choice of JSPE was related to its specificity for the medical student in a medical context, and the IRI-Brazilian version due to its multidimensional component, which assesses both the affective and cognitive dimensions of empathy.
The Jefferson Scale of Physician Empathy (JSPE) evaluates the cognitive dimension of empathy. It consists of 20 questions that are answered using the Likert scale of 7 points (1=strongly disagree, 7=strongly agree). The scores obtained for each question will be added together, resulting in a final score for empathy. Questions 1, 3, 6, 7, 8, 11, 12, 14, 18 and 19 have a reverse score.
The IRI-Brazilian version developed by Davis consists of 21 items that assess the cognitive and affective dimensions of empathy. The answer is given on a 5-point Likert scale (from 1=“doesn’t describe me very well” to 5=“describes me very well”). The answers to questions 2, 3, 9, 10, 11 and 13 have a reverse score. The values obtained for each question will be added to the final score and dimension (cognitive and affective).
An isolated analysis was carried out of the mean Jefferson Scale scores, IRI-Brazilian version and subscales affective and cognitive dimension. For this analysis, the scores of each scale, from zero to 100 points were standardized and then compared to the average. This standardization was performed using the following formula:
- •
Study variablesFrom each participant, we obtained socio-demographic data: gender, year/semester of medical school, and the field of specialization the student was interested in. The specializations were classified in groups (“Clinic”, “Surgery” and “Other”)
- •
Statistical analysisThe students were divided into 3 groups according to their year of graduation: “Basic” (1st and 2nd years), “Clinical” (3rd and 4th years) “Clerkship” (5th and 6th years). The socio-demographic data and empathy scores of both scales were compared between these 3 groups using the Chi-square test and the Kruskal–Wallis test, where applicable.We performed multiple linear regression models to assess the association between empathy scores according to year group (basic, clinical and clerkship). The models presented are crude and are adjusted for gender and intended specialty.
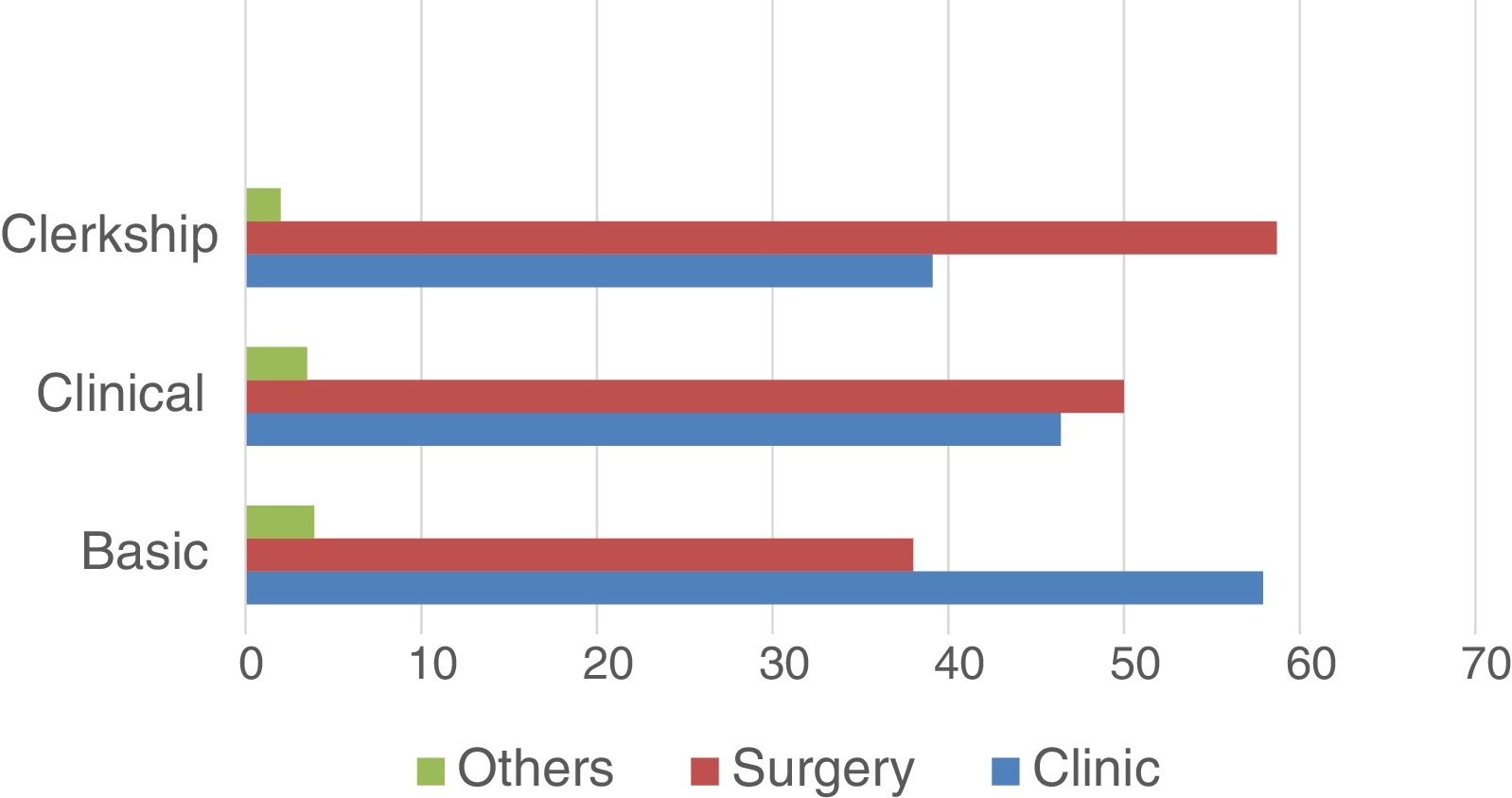
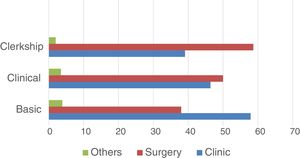
Of the total of 577 medical students at the University studied, 296 (51%) participated in this study. Graphic 1 shows the field of specialization the student was interested in according to the year of graduation (Basic – 1st and 2nd years, Clinical – 3rd and 4th years and Clerkship – 5th and 6th years).
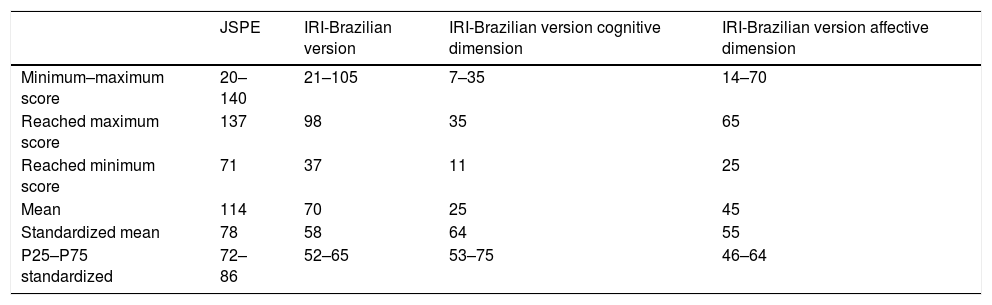
Comparing the standardized averages of the two scales scores, we identified a significant difference between them, with the lowest average being obtained for the affective dimension of empathy. Table 1 shows the maximum and minimum values of the scores obtained on each scale, as well as the standardized average.
Scores of empathy scales and standardized mean.
| JSPE | IRI-Brazilian version | IRI-Brazilian version cognitive dimension | IRI-Brazilian version affective dimension | |
|---|---|---|---|---|
| Minimum–maximum score | 20–140 | 21–105 | 7–35 | 14–70 |
| Reached maximum score | 137 | 98 | 35 | 65 |
| Reached minimum score | 71 | 37 | 11 | 25 |
| Mean | 114 | 70 | 25 | 45 |
| Standardized mean | 78 | 58 | 64 | 55 |
| P25–P75 standardized | 72–86 | 52–65 | 53–75 | 46–64 |
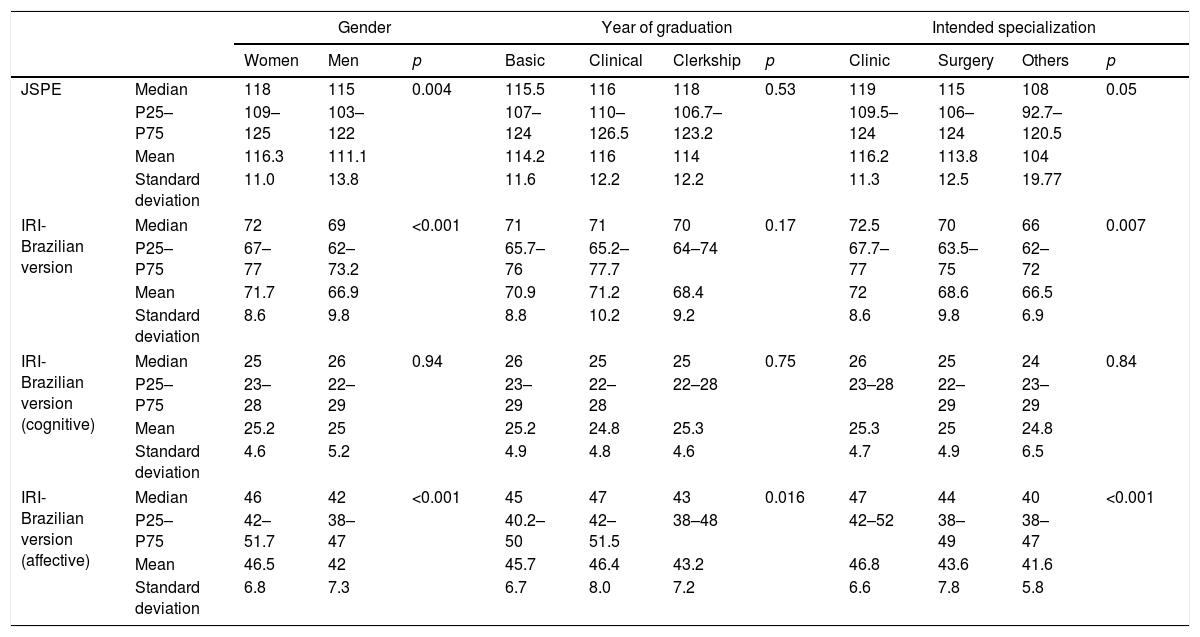
Analyzing the empathy score, we found a significant decrease in empathy score in the affective dimension of IRI-Brazilian version in the Clerkship group (p=0.016) (Table 2). The scores for the JSPE, IRI-Brazilian version and IRI-Brazilian version cognitive dimension showed no significant changes in the scores among the groups.
Compare empathy score according to gender, year of graduation, and intended specialization.
| Gender | Year of graduation | Intended specialization | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Women | Men | p | Basic | Clinical | Clerkship | p | Clinic | Surgery | Others | p | ||
| JSPE | Median | 118 | 115 | 0.004 | 115.5 | 116 | 118 | 0.53 | 119 | 115 | 108 | 0.05 |
| P25–P75 | 109–125 | 103–122 | 107–124 | 110–126.5 | 106.7–123.2 | 109.5–124 | 106–124 | 92.7–120.5 | ||||
| Mean | 116.3 | 111.1 | 114.2 | 116 | 114 | 116.2 | 113.8 | 104 | ||||
| Standard deviation | 11.0 | 13.8 | 11.6 | 12.2 | 12.2 | 11.3 | 12.5 | 19.77 | ||||
| IRI-Brazilian version | Median | 72 | 69 | <0.001 | 71 | 71 | 70 | 0.17 | 72.5 | 70 | 66 | 0.007 |
| P25–P75 | 67–77 | 62–73.2 | 65.7–76 | 65.2–77.7 | 64–74 | 67.7–77 | 63.5–75 | 62–72 | ||||
| Mean | 71.7 | 66.9 | 70.9 | 71.2 | 68.4 | 72 | 68.6 | 66.5 | ||||
| Standard deviation | 8.6 | 9.8 | 8.8 | 10.2 | 9.2 | 8.6 | 9.8 | 6.9 | ||||
| IRI-Brazilian version (cognitive) | Median | 25 | 26 | 0.94 | 26 | 25 | 25 | 0.75 | 26 | 25 | 24 | 0.84 |
| P25–P75 | 23–28 | 22–29 | 23–29 | 22–28 | 22–28 | 23–28 | 22–29 | 23–29 | ||||
| Mean | 25.2 | 25 | 25.2 | 24.8 | 25.3 | 25.3 | 25 | 24.8 | ||||
| Standard deviation | 4.6 | 5.2 | 4.9 | 4.8 | 4.6 | 4.7 | 4.9 | 6.5 | ||||
| IRI-Brazilian version (affective) | Median | 46 | 42 | <0.001 | 45 | 47 | 43 | 0.016 | 47 | 44 | 40 | <0.001 |
| P25–P75 | 42–51.7 | 38–47 | 40.2–50 | 42–51.5 | 38–48 | 42–52 | 38–49 | 38–47 | ||||
| Mean | 46.5 | 42 | 45.7 | 46.4 | 43.2 | 46.8 | 43.6 | 41.6 | ||||
| Standard deviation | 6.8 | 7.3 | 6.7 | 8.0 | 7.2 | 6.6 | 7.8 | 5.8 | ||||
Comparing the empathy scores according to gender (men and women), we identified that women have higher empathy scores than men (p<0.01 for IRI-Brazilian version affective dimension, IRI-Brazilian version and JSPE scores), but not for the cognitive component of IRI-Brazilian version scale (p=0.94) (Table 2).
In the bivariate analysis, the JSPE, IRI-Brazilian version, and IRI-Brazilian version affective dimension scores were higher for students wishing to specialize in clinical specialties. In terms of intended specialty, there was no significant difference when using the cognitive dimension of the IRI-Brazilian version (Table 2).
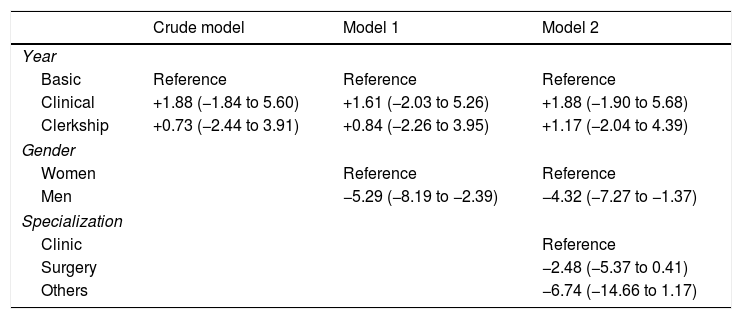
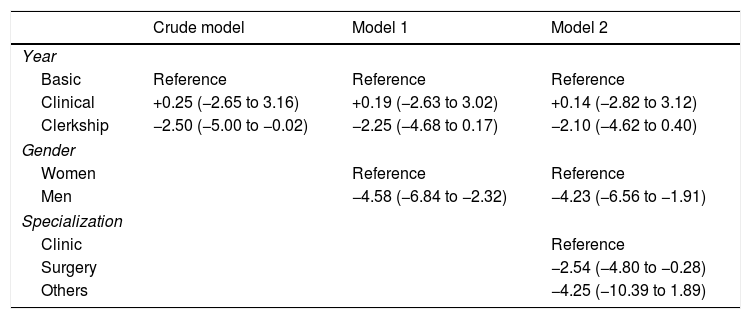
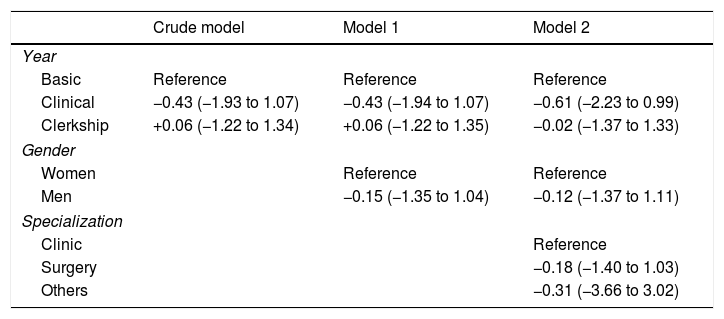
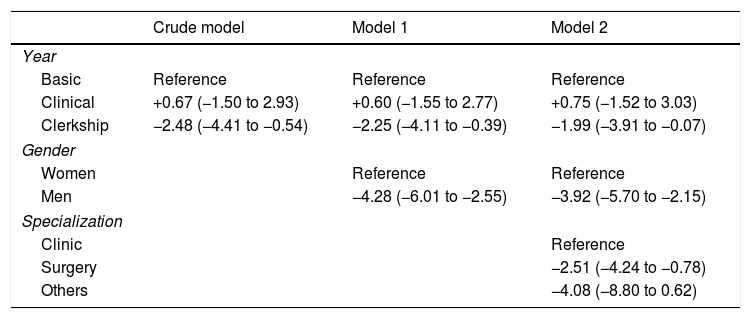
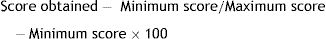
Tables 3–6 show the results of the linear regression models. In the adjusted models, the JSPE scores were not significantly associated with the year of medical course or intended specialty. Men had lower empathy scores compared to women in the adjusted models. Analyzing the IRI-Brazilian version scores, we found lower scores in the clerkship group in the crude models, but this difference vanished after adjustment for gender. The full models showed lower scores in men and in those who intended to follow surgical careers. Analyzing the IRI-Brazilian version affective dimension score, the clerkship group, men, and those who intended to follow surgical careers were associated with lower scores in the full-adjusted models. The IRI-Brazilian version cognitive dimension scores showed no significant differences according to year of graduation, gender or intended specialization.
Beta coefficients (95% confidence interval) associated with the score obtained in the JSPE empathy scale.
| Crude model | Model 1 | Model 2 | |
|---|---|---|---|
| Year | |||
| Basic | Reference | Reference | Reference |
| Clinical | +1.88 (−1.84 to 5.60) | +1.61 (−2.03 to 5.26) | +1.88 (−1.90 to 5.68) |
| Clerkship | +0.73 (−2.44 to 3.91) | +0.84 (−2.26 to 3.95) | +1.17 (−2.04 to 4.39) |
| Gender | |||
| Women | Reference | Reference | |
| Men | −5.29 (−8.19 to −2.39) | −4.32 (−7.27 to −1.37) | |
| Specialization | |||
| Clinic | Reference | ||
| Surgery | −2.48 (−5.37 to 0.41) | ||
| Others | −6.74 (−14.66 to 1.17) | ||
The independent variables in adjusted model 1 are year (basic, clinical and clerkship) and gender.
The independent variables in adjusted model 2 are year (basic, clinical and clerkship), gender and intended specialization.
Beta coefficients (95% confidence interval) associated with the score obtained in the IRI-Brazilian version.
| Crude model | Model 1 | Model 2 | |
|---|---|---|---|
| Year | |||
| Basic | Reference | Reference | Reference |
| Clinical | +0.25 (−2.65 to 3.16) | +0.19 (−2.63 to 3.02) | +0.14 (−2.82 to 3.12) |
| Clerkship | −2.50 (−5.00 to −0.02) | −2.25 (−4.68 to 0.17) | −2.10 (−4.62 to 0.40) |
| Gender | |||
| Women | Reference | Reference | |
| Men | −4.58 (−6.84 to −2.32) | −4.23 (−6.56 to −1.91) | |
| Specialization | |||
| Clinic | Reference | ||
| Surgery | −2.54 (−4.80 to −0.28) | ||
| Others | −4.25 (−10.39 to 1.89) | ||
The independent variables in adjusted model 1 are year (basic, clinical and clerkship) and gender.
The independent variables in adjusted model 2 are year (basic, clinical and clerkship), gender and intended specialization.
Beta coefficients (95% confidence interval) associated with the score obtained in the IRI-Brazilian version cognitive dimension.
| Crude model | Model 1 | Model 2 | |
|---|---|---|---|
| Year | |||
| Basic | Reference | Reference | Reference |
| Clinical | −0.43 (−1.93 to 1.07) | −0.43 (−1.94 to 1.07) | −0.61 (−2.23 to 0.99) |
| Clerkship | +0.06 (−1.22 to 1.34) | +0.06 (−1.22 to 1.35) | −0.02 (−1.37 to 1.33) |
| Gender | |||
| Women | Reference | Reference | |
| Men | −0.15 (−1.35 to 1.04) | −0.12 (−1.37 to 1.11) | |
| Specialization | |||
| Clinic | Reference | ||
| Surgery | −0.18 (−1.40 to 1.03) | ||
| Others | −0.31 (−3.66 to 3.02) | ||
The independent variables in adjusted model 1 are year (basic, clinical and clerkship) and gender.
The independent variables in adjusted model 2 are year (basic, clinical and clerkship), gender, and intended specialization.
Beta coefficients (95% confidence interval) associated with the score obtained in the IRI-Brazilian version affective dimensions.
| Crude model | Model 1 | Model 2 | |
|---|---|---|---|
| Year | |||
| Basic | Reference | Reference | Reference |
| Clinical | +0.67 (−1.50 to 2.93) | +0.60 (−1.55 to 2.77) | +0.75 (−1.52 to 3.03) |
| Clerkship | −2.48 (−4.41 to −0.54) | −2.25 (−4.11 to −0.39) | −1.99 (−3.91 to −0.07) |
| Gender | |||
| Women | Reference | Reference | |
| Men | −4.28 (−6.01 to −2.55) | −3.92 (−5.70 to −2.15) | |
| Specialization | |||
| Clinic | Reference | ||
| Surgery | −2.51 (−4.24 to −0.78) | ||
| Others | −4.08 (−8.80 to 0.62) | ||
The independent variables in adjusted model 1 are year (basic, clinical and clerkship) and gender.
The independent variables in adjusted model 2 are year (basic, clinical and clerkship), gender and intended specialization.
We found that women obtained better scores for empathy compared to men, in both scales. Only in IRI-Brazilian version cognitive dimension was there no difference between genders. These findings related to gender were the same as identified in studies by Hojat et al.,6 Davis,20 Eisenberg et al.,26 Hasan et al.,27 Mandel et al.,28 Hojat et al.29
About specialty, students intending to follow clinical careers had higher empathy scores, compared to those intending to follow a surgical career. The same results were found in studies by Hojat et al.,6 Coutts-van Dijk et al.,30 Bailey.31
We would like to focus our discussion on another important finding, which was the possible affective erosion among students during medical school.
The results of this study demonstrate an important and challenging point in medical education, which is the medical student's affection. In all the statistical analyses, lower scores were obtained in the Clerkship group for the affective dimension of empathy assessed by the IRI-Brazilian version, suggesting that the affective dimension is the most affected during medical school. When we compared the scores of the JSPE and IRI-Brazilian version, the lowest score was obtained for the affective dimension of the IRI-Brazilian version, highlighting the importance of discussion on the subject of education in affection during medical school.
The universe of affection, feelings and emotions has had a leading role in the educational environment. The classical pedagogical approach usually divides the educational objectives into three broad categories: cognitive, psychodynamic, and the education of affection. There is no way to objectively measure the growth or correct affective dynamic guidance of the student. In this context, it is more difficult to measure the danger of being forgotten, or placed under the purely arbitrary. Most of the time, the assessment of affective education is not taken into account when establishing educational objectives.32
Educating emotions implies a serious process, which should initially be identified and then make them explicit and able to be worked by the teacher aiming to be used properly to promote effective patient doctor relationship. This educational process of educating affection requires tact, skill, avoid precipitation, promote learning to respect in any way, the physiological rhythm of emotion. You cannot force anyone to feel what one does not feel. What one can do is wait for a time of reflection over what one may feel, and from there develop affection, which is a true education process.33
The emotions play an important role in the lives of medical students. They have to deal not only with their own emotions, but also with those of their patients. However, few components of their formal graduation are focused on their emotional lives.34
A fact that supports this finding occurs when the student is exposed to medical practice during the clerkship (5th to 6th years). During this period, there is a predominant culture of keeping a certain distance from the patient, and avoiding emotional involvement. This behavior can be seen as a defense mechanism, a desire to distance oneself from the suffering of others, or a desire to avoid a sense of powerlessness over the situation.35 When professionals, whether students or doctors, wrongly seek to protect their emotions under a cloak of impersonality, empathy is compromised.
It is understandable that without adequate preparation, medical students may express inappropriate emotional responses to situations commonly encountered in medical practice, such as pain, suffering and death – situations that make them aware of their own vulnerability.36 When the student does not have the opportunity to work through their emotions, and to reflect and to share the feelings generated by them, they may develop an emotional detachment, seeking support based purely on their biomedical skills. But training in biomedical knowledge is given too much emphasis, merely drawing students further away from the humanist and ethical behavior that is always preferable.37
To be empathic, it is necessary to see and understand the patient's suffering, and also to understand one's own reactions to the patient's suffering.38 The exercise of self-critical reflection on the encounter with the patient, together with an understanding of one's own emotions, is a prerequisite to understanding the feelings of others, and is therefore an indicator of empathic ability.39
Intervention possibilitiesBayne40 highlights the importance of teacher education in this model of empathy process. It is essential for the development of empathy that the student experience empathic relationships with their teachers. This way, the student is more likely to develop an empathetic relationship with their patients.
Borrell41 strengthens the role of the teacher, stating that learning takes place through the “spread” of ethical attitudes from the teacher, demonstrated during their daily clinical practice.
There is a close relationship between life experiences and the development of empathy. Hence, the importance of learning by example, in an educational learning setting where medical students and young people are inspired by the attitudes of their teachers during practice with the patient. This model, which English-speaking educators call “tag-along”, allows students to incorporate attitudes and behaviors in their approach to real patients, and to identify useful questions for their professional careers.42
Beyond the example of the teacher, teaching and promoting empathy has the possibilities arising from humanistic and cultural training. The art that imitates life, offers diverse needs where the student is able to incorporate the features “hard to teach” (by traditional methods). Hence some authors emphasize the importance of art, literature and reflection in the student's own life, for the development of empathy.36
The main goal of incorporating the humanities into medical education is to awaken attitudes and values that are often unexpected in the students themselves, who rely on the scale of values, education and maturity that each possesses. The objectives are measured not so much by the final results, as the enlarged capacity of understanding of the human being that the process gives them, including what are called latent results.
Music has been shown to be a useful tool for enabling medical students to talk about themselves, ask questions, and discuss their expectations as a future doctor. It also helps revive ideals, dreams and life values.43 The education of affectivity using film has also shown positive results in stimulating reflection among medical students.44 Reflection is critical for the improvement of attitudes and behavior, as well as the incorporation of virtues and values.
Other instruments have also shown promising results in addressing issues related to the student's emotions, such as the use of literature, narratives45 and opera.46
Strengths and limitations of the studyThis study is the application of consolidated fortress scales in the literature, which allows comparability with other studies. It also has some limitations, such as its single-center design, which affect the generalization and cross-sectional analysis. This enables the study of putative associations but impairs causal inference. Nevertheless, our findings of a trend toward lower empathy scores in the final years of graduation (statistically significant in IRI-Brazilian version affective dimension score) is consistent with the results of a longitudinal study by Hojat et al.,6 which identified an erosion of empathy during the medical course.
ConclusionOur research suggests that the level of empathy can change and in this case, the affective dimension was the most affected during medical school. The identification of affective erosion strengthens the need to develop effective educational strategies that contribute to a good training medical for the professional future.
Conflict of interestThe authors of this article declare no conflict of interest.