Several studies show a high prevalence of burnout among medical students, with the learning environment being suggested as one of the potential contributing factors. The present analysis aims to describe burnout in medical students and its relationship with the educational climate.
We have investigated the relationship between burnout and academic climate. Previously, we found a correlation between a poor perception of academic climate with increased depression, anxiety, and other psychopathological symptoms.
Material and methodsThe study was carried out in 2022 in all 44 medical schools in Spain and analyses the academic climate (Dundee Ready Education Environment Measure) and its relationship with the perception of burnout (Maslach Burnout Inventory) among medical students (n=4374).
ResultsThe global academic climate and the burnout subscales present an inverse correlation with exhaustion and depersonalization, and a direct correlation with efficacy. Students in public schools presented greater values for exhaustion and depersonalization than those from private centers. The levels of burnout increase during the stay in the school in these 3 subscales.
ConclusionOur study suggests a high correlation between a higher level of burnout and a worse assessment of the academic climate. The level of burnout varies according to gender, course, and type of medical school.
Varios estudios muestran una alta prevalencia de agotamiento entre los estudiantes de medicina, sugiriendo el entorno de aprendizaje como uno de los posibles factores contribuyentes. El presente análisis tiene como objetivo describir el burnout en estudiantes de medicina y su relación con el clima educativo.
Material y métodosEl estudio se llevó a cabo en 2022 en las 44 facultades de medicina de España y analiza el clima académico (Dundee Ready Education Environment Measure) y su relación con la percepción del burnout (Maslach Burnout Inventory) entre los estudiantes de medicina (n=4374).
ResultadosEl Clima Académico Global y las subescalas de burnout presentan correlación inversa con Agotamiento y Despersonalización, y correlación directa con Eficacia. Los estudiantes de centros públicos presentaron mayores valores de agotamiento y despersonalización que los de centros privados. Los niveles de burnout aumentan durante la estancia en el centro educativo en estas tres subescalas.
ConclusiónNuestro estudio sugiere una alta correlación entre un mayor nivel de burnout y una peor valoración del clima académico. El nivel de agotamiento varía según el género, la carrera y el tipo de escuela de medicina.
Several investigations have shown significantly high levels of stress and burnout in medical students throughout their university career.1–9 Among them, several systematic reviews2,3 indicate that approximately half of medical students in the United States experience symptoms of burnout. In Spain, one of the first studies carried out by Galán et al.5 showed that as the grade progresses, burnout increases, doubling the scores of students in the sixth course compared to the third year. In this study, no relationship was found between burnout and gender. Later studies found similar figures for burnout, as well as its increase during grade.6–8
The term burnout is initially described by Freudenberger and conceptualized by Maslach,10 who defines it as a combination of 3 factors: emotional exhaustion (EE) in reference to psychological exhaustion; depersonalization and cynicism (DP), which is initially established as a defense mechanism and evolves into an indifferent and apathetic relationship towards patients and colleagues; and personal fulfillment (PR), which implies a decreased sense of personal achievement and perception of work inefficiency. Maslach describes the development of burnout as a continuum between these factors: it begins with emotional and physical exhaustion and as EE becomes more continuous, DP, with a negative attitude, would appear. The third component, lack of PR, would appear later with feelings of incompetence, helplessness, and decreased productivity even in the face of positive results. In students, burnout syndrome is shown by a lack of concentration and attention, difficulty retaining information, a feeling of fatigue and helplessness, or lack of ability to make an effort.1,7,8
Burnout is associated with worse mental health and suicidal ideation and there is a correlation between poor mental health during the student period, during residency, and during professional practice. A correlation has also been shown between burnout (especially with the factors EE and depersonalization) and alcohol abuse or dependence.4 The consequences of a higher level of burnout are important; it has been related to worse academic performance,6,9 greater academic dishonesty,11 lower professional values12 with less empathy, greater cynicism, and less willingness to serve.13,14 Factors related to the development of burnout in medical students are identified as factors such as academic pressure,15 workload,16 exposure to death and suffering of the patient,17 and the “hidden curriculum”.18–20 Predisposing factors of a personal nature are also described, such as lack of coping strategies for stress, very high motivation, exaggerated sense of responsibility and idealization of work, or resistance to requesting help.20
Some studies also suggest that there is a great influence of factors related to the learning environment as promoters of burnout, more than individual characteristics.21–23 Academic climate measures social interaction, organizational culture and structures, and students' experiences, perceptions, and learning. A better academic climate is associated with better quality of life21 and lower burnout.3,4,22 In a previous study, we have shown that a poor perception of academic climate is correlated with increased depression, anxiety, and other psychopathological symptoms, with a pattern that varies between different faculties.23 The present analysis aims to describe burnout in medical students and its relationship with the educational climate.
Material and methodsThis is a cross-sectional multicenter study. All medical degree students from the 44 medical schools in Spain during 2022 were included. It was developed through an anonymous survey in a web questionnaire in Google Forms. The participants, all medical students, were recruited through text messages sent by the Student Delegations of each school. Part of the data of this study has been already presented in a previous paper.32 Participation was voluntary and students gave informed consent before completing the survey. The questionnaires used were:
- •
Maslach Burnout Inventory Student Survey Questionnaire: developed by Schaufeli et al.,24 it is an academic burnout questionnaire adapted to students derived from the Maslach Burnout Inventory. It measures 3 factors: exhaustion, cynicism, and academic efficacy (as opposed to the ineffectiveness implied by burnout). It has 15 items evaluated on a 7-point Likert scale (from 0 to 6). High burnout implies high scores on the exhaustion and cynicism scales and low scores on the academic efficacy scale. A total score is also calculated by inverting the Effectiveness scale and transforming it into Ineffectiveness.
- •
Dundey Ready Education Environment Measure (DREEM): The main variable was the educational climate that was measured using the valid version given in Spanish from the DREEM questionnaire.25,26 The DREEM consists of 50 items that can be assessed on a 5-point Likert-type scale. The items are classified into 5 subscales: students' perception of learning, students' perception of teachers, students' academic self-perception, students' perception of the atmosphere, and students' social self-perception. The maximum score that can be achieved in this questionnaire is 200 points and, in the guide, to using this questionnaire, and in previous studies carried out, the following relationship between the overall results obtained and the quality of the educational climate has been considered: 0–50 very poor; 51–100 existence of many problems; 101–150 more positive than negative; 151–200 excellent. The DREEM also allows us to identify the strengths and weaknesses of the teaching curriculum.
Descriptive statistics have been calculated and the comparison of means has been carried out using Student's t test. For the relationship between quantitative variables, the Pearson correlation coefficient is used. All analyzes have been carried out bilaterally and with a statistical significance of 0.05, using the JAMOVI 2.2.5 program.
Results4433 students from 46 Spanish Medical Faculties participated in the study. The participants were 3319 female students (74.9%), 1080 men (24.4%), and 34 non-binary students (0.8%). The mean age was 21.5 years (SD 3.52). Participation by course has been 19.3% in the first year, 17.6% in the second year, 19.6% in the third year, 17.6% in the fourth year, 16.0% in the fifth year, and 9.9% in the sixth year.
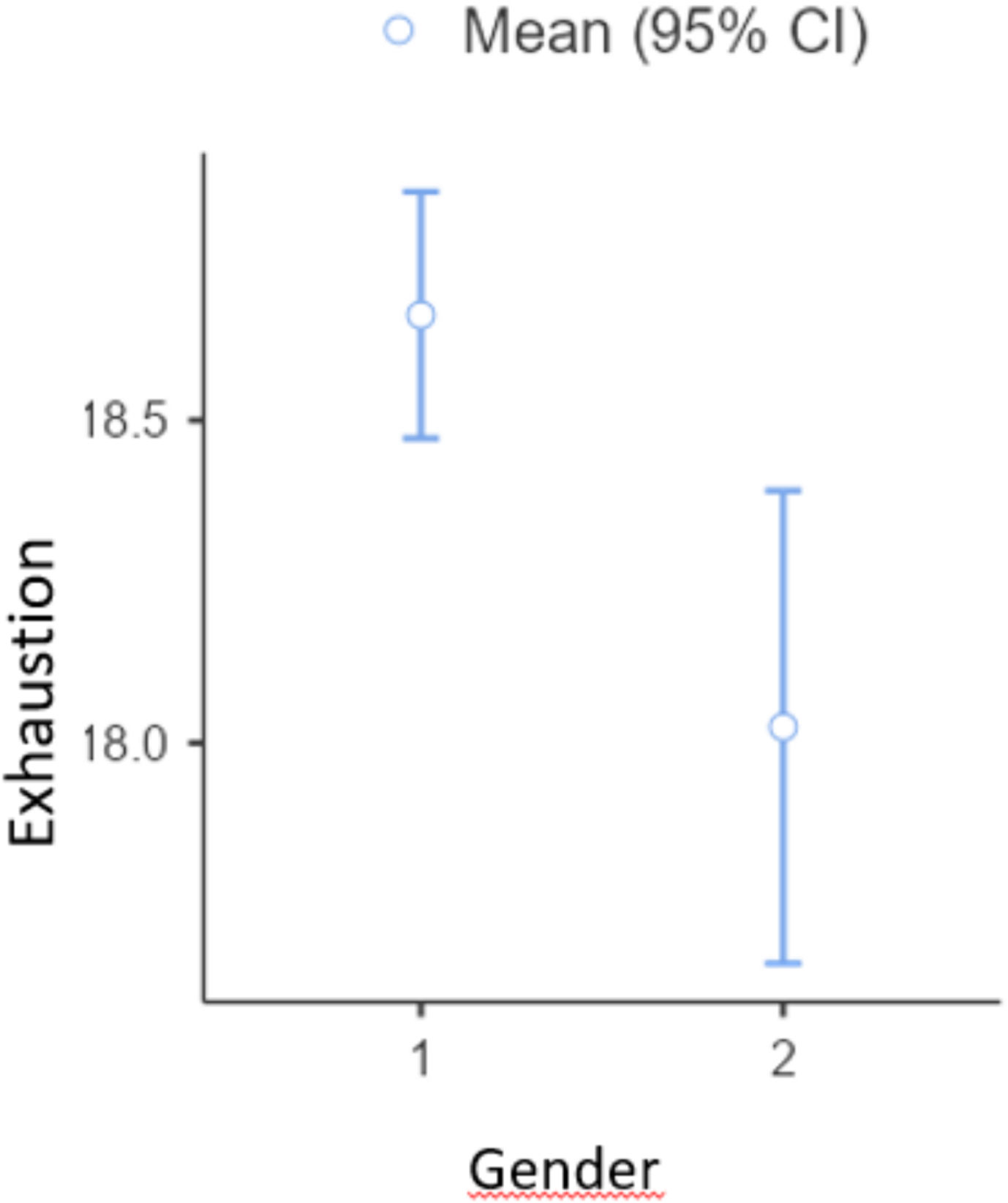
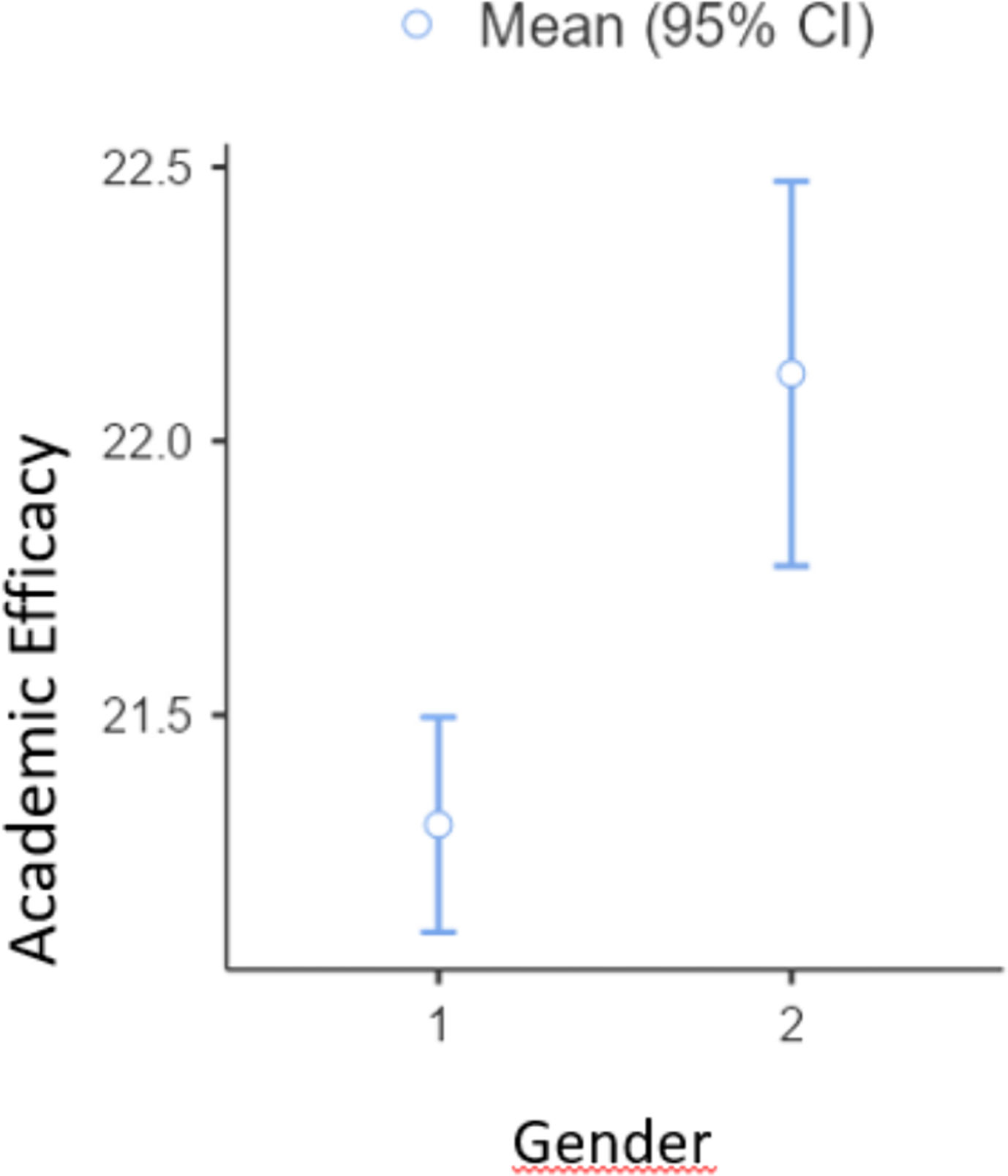
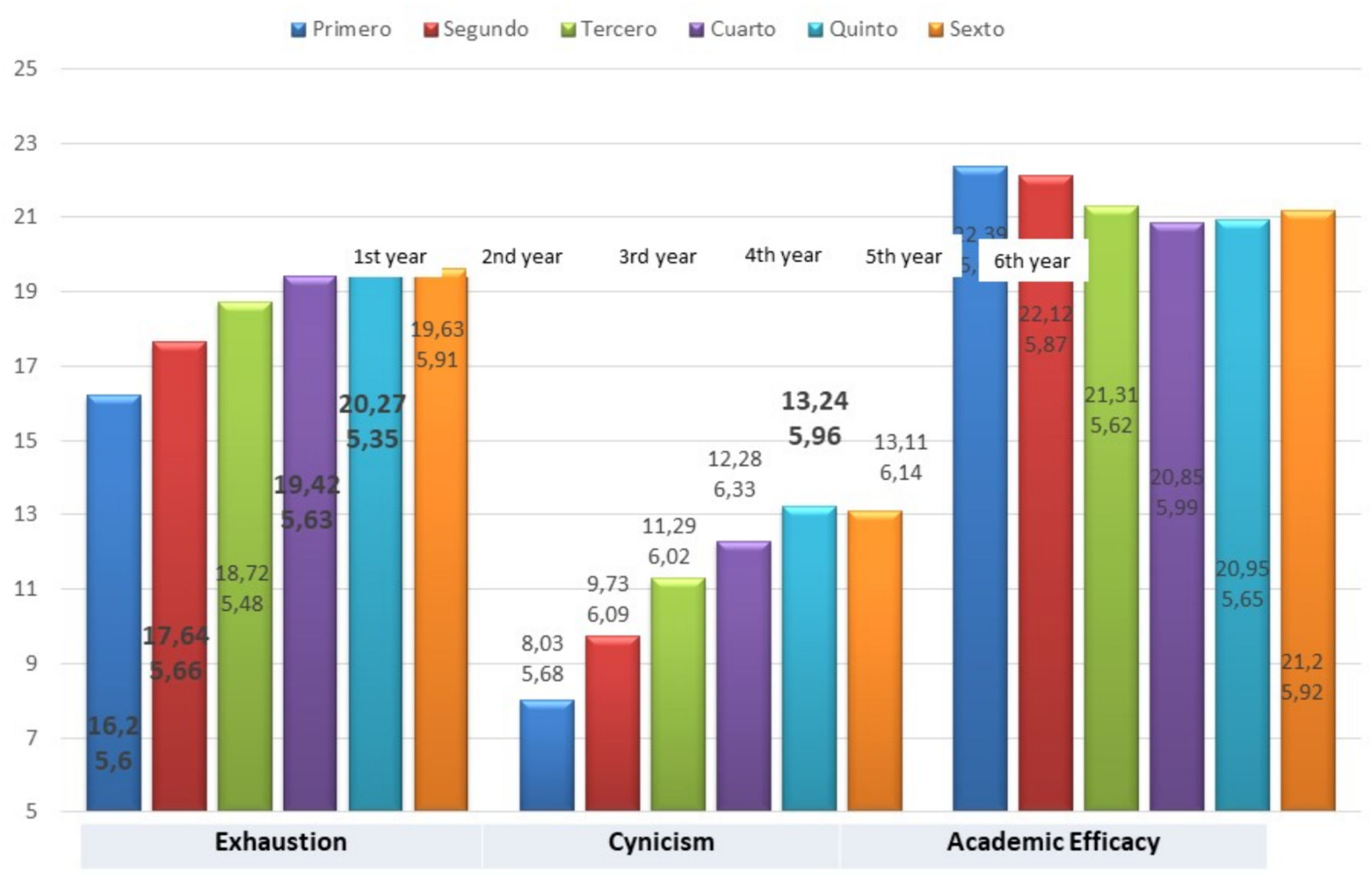
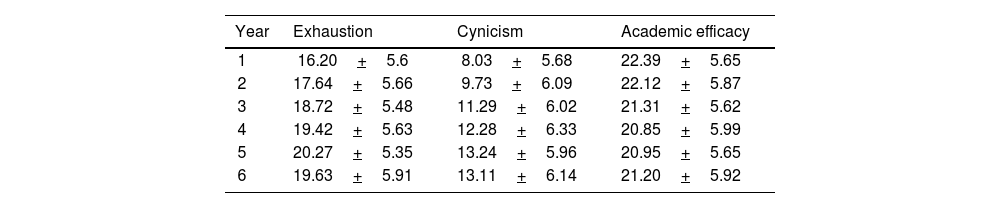
In relation to the burnout figures, the results present a mean of 18.5 (SD 5.75) in the exhaustion subscale; mean 11.1 (SD 6.31) on the cynicism or depersonalization subscale; and mean 21.5 (SD 5.8) on the academic efficacy subscale. The burnout scores in the moderate–high exhaustion subscale (>21.2) were 68.2% and in the depersonalization subscale the moderate-high score occurred in 27.1%. In relation to gender, female students present higher levels of exhaustion (t 3.16, p=.002) and lower levels of academic efficacy (t −4.05, p<.001) (Figs. 1 and 2). In relation to age, the older the person, the higher the levels of burnout in the 3 subscales: exhaustion (P 0.18, p<.001), depersonalization (P 0.19, p<.001), and efficacy (P 0.06, p<.001). Table 1 and Fig. 3 show the burnout figures according to the academic year.
Burnout subscales in every year in medical school (data are mean+standard deviation).
| Year | Exhaustion | Cynicism | Academic efficacy |
|---|---|---|---|
| 1 | 16.20+5.6 | 8.03+5.68 | 22.39+5.65 |
| 2 | 17.64+5.66 | 9.73+6.09 | 22.12+5.87 |
| 3 | 18.72+5.48 | 11.29+6.02 | 21.31+5.62 |
| 4 | 19.42+5.63 | 12.28+6.33 | 20.85+5.99 |
| 5 | 20.27+5.35 | 13.24+5.96 | 20.95+5.65 |
| 6 | 19.63+5.91 | 13.11+6.14 | 21.20+5.92 |
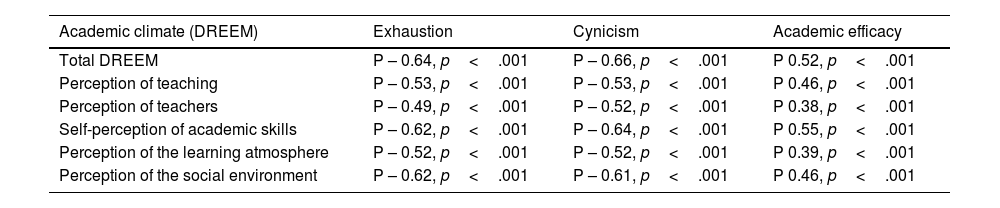
Students from public school, compared to private centers, presented higher levels of Exhaustion (t 6.6, p<.001), greater depersonalization (t 8.6, p<.001), and lower levels of academic efficacy (t −9.2, p<.001). The figures for global academic climate and all its subscales present an inverse correlation with exhaustion and depersonalization, and a direct correlation with Efficacy, as shown in Table 2.
Correlation between academic climate and burnout (Pearson p).
| Academic climate (DREEM) | Exhaustion | Cynicism | Academic efficacy |
|---|---|---|---|
| Total DREEM | P – 0.64, p<.001 | P – 0.66, p<.001 | P 0.52, p<.001 |
| Perception of teaching | P – 0.53, p<.001 | P – 0.53, p<.001 | P 0.46, p<.001 |
| Perception of teachers | P – 0.49, p<.001 | P – 0.52, p<.001 | P 0.38, p<.001 |
| Self-perception of academic skills | P – 0.62, p<.001 | P – 0.64, p<.001 | P 0.55, p<.001 |
| Perception of the learning atmosphere | P – 0.52, p<.001 | P – 0.52, p<.001 | P 0.39, p<.001 |
| Perception of the social environment | P – 0.62, p<.001 | P – 0.61, p<.001 | P 0.46, p<.001 |
In this cross-sectional survey carried out among medical students, a significant correlation was observed between a higher degree of burnout and an unfavorable perception of the academic climate. As appears in previous studies, the degree of burnout is high and increases during medical courses.1–8 In our sample, a relationship appears between burnout and gender, in the EE and efficacy subscales. In the literature, some studies show a relationship between burnout and gender in medical students on some scales, while other studies do not show a difference.3–7 Studies that show a higher risk of burnout in women in the context of medical education attribute it to factors such as differences in social expectations, gender roles, the additional burden associated with multiple responsibilities, or differences in coping strategies according to gender.1–3
Regarding the type of university centers, private schools showed a lower degree of burnout on all scales. No similar studies have been found in our environment, but in other territorial areas, greater burnout is described in private universities, linked to economic pressure.27-29 Medical students who perceived the learning environment less favorably were more likely to develop higher levels of burnout on all 3 scales: exhaustion, cynicism, and low self-efficacy, than medical students with more positive perceptions of the academic climate.
Previous studies21,29,30 suggest that the academic climate influences several factors in the development of burnout. The environment covers various aspects, from the academic context to interpersonal relationships and socioeconomic conditions. Some of the environmental factors what could contribute to burnout in medical students are pressure and academic demands; the institutional culture with a competitive, uncollaborative, or lack of support environment; interpersonal relationships with classmates and teachers; access to resources; or the balance between study and personal life.29,30
Burnout has been defined at a clinical level as a hidden health crisis due to its high impact on both a personal and healthcare level, and it could also be defined as a hidden academic crisis. We know that there is a continuum between academic burnout and subsequent professional development, so it is essential that medical schools consider and promote the well-being of their students.2 Previous studies suggests that specific modifiable aspects of the learning environment are related to variations in academic burnout. Specific interventions in the academic climate have been described as associated with better emotional well-being among medical students, but the same authors recognize that higher quality studies are necessary to corroborate this statement.29 The environment in which medical students operate plays a role in the appearance of burnout. Creating academic environments that promote mental health, offer emotional support, and facilitate balance between academic demands and personal life may be crucial to preventing or mitigating burnout in these students.
As limitations, the choice to use a self-administered instrument instead of structured clinical interviews could also be considered a limitation and in addition, there is the possibility that those students more sensitive to these issues or aware of their own problems were more inclined to participate in the survey compared to others. The national breadth of the design provides a perspective of generalization of the results. However, it is important to note that, despite the high number of responses, the applicability of the findings may vary between different universities, given that the response rate differed significantly between centers. Finally, it is crucial to note that the sampling procedure was non-probabilistic, as participation was offered to everyone, but only those interested chose to participate.
This study represents the initial examination of the correlation between these factors within our country. It serves as a foundational step for future research endeavors aimed at further understanding the influences on both the perception of an unfavorable academic climate and the manifestation of burnout. Moreover, it seeks to delineate the characteristics of students who are at higher risk.
In conclusion, our study suggests a high correlation between a higher level of burnout and a worse assessment of the academic climate. The level of burnout varies according to gender, course, and type of medical school. Additional research is needed to detect which specific modifiable aspects of the learning environment are strongly related to burnout and poor mental health, as well as determine the best strategies to create and maintain a learning environment that cultivates students' professional development.
Ethical approvalThe study was approved by the Ethics Committee of the University of Murcia (reference 3772/2022) in accordance with the Spanish Medical Research with Human Subjects law. Informed consent was obtained from the study participants. Participation in this anonymous questionnaire was voluntary and participants could refuse to participate or discontinue participation at any time without penalty. The anonymous questionnaires could not be traced back to individuals. Data were stored on secure servers and only people involved in this study had access to it. All methods were performed in accordance with relevant guidelines and regulations.
Conflicts of interestJoaquín García-Estañ and Jesús Millán are part of the Editorial Board of Educacion Medica Journal and declare that they have remained outside the evaluation and decision-making process regarding this article. The other authors declare that they have no conflicts of interest.
FundingThe authors declare that no funding was received for this article.