Stress factors influence surgical procedures. This study aims to assess the impact of stress factors on surgical performance in ophthalmology simulation. Specifically, the study aims to identify which exercises are most affected by stress and to examine the relationship between stress levels, surgical complexity, and technical skills.
Material and methodsA prospective study of a cohort of 13 ophthalmology residents, at Vall Hebron University Hospital. All study participants received basic training before the study to become familiar with the simulator and surgical maneuvers. Once completed, the participants were invited to perform 3 defined exercises (E1, E2, and E3, increasing difficulty level from 1 to 3) in relaxed conditions. Afterwards, the same exercises were performed again under a stressful environment. The stress was created introducing physical, auditory, and interruptions factors. The results in technical skills were evaluated through the relaxation and stress scores, as well as the time required to complete the exercises under relaxation and stress conditions. A detailed metric was used to assess the variables in relation to stress situations, including physical stress, haste, the presence of background music, and scheduled interruptions.
The results are expressed by median and interquartile range. To compare them, Wilcoxon test for paired samples and the Whitney U Test were performed. The results were stratified by year of residence (1–2 years vs 3–4 years).
ResultsThe stress score was significantly lower in the 3 exercises compared to the relax score (75 vs 86, 52 vs 90, 55 vs 61, respectively, p>.05). Time to perform the exercises was less predictable and was even lower in stressful situations with no statistical differences. Under stress, both younger and older residents scored worse on the more complex exercises.
ConclusionStress affects surgery with simulators. The most difficult exercises are the most likely to be affected by stress. These results suggest that through ophthalmic simulators ophthalmologists have the opportunity to train surgical stress and therefore improving patient safety.
Los factores de estrés influyen en los procedimientos quirúrgicos. Este estudio tiene como objetivo evaluar el impacto de los factores de estrés en el desempeño quirúrgico en simulaciones oftalmológicas. Específicamente, el estudio busca identificar qué ejercicios se ven más afectados por el estrés y examinar la relación entre los niveles de estrés, la complejidad quirúrgica y las habilidades técnicas
Materiales y métodosEstudio prospectivo de una cohorte de 13 residentes de oftalmología en el Hospital Universitario Vall Hebron. Todos los participantes del estudio recibieron entrenamiento básico antes del estudio para familiarizarse con el simulador y las maniobras quirúrgicas. Una vez completado, se invitó a los participantes a realizar tres ejercicios definidos (E1, E2, E3, aumentando el nivel de dificultad de 1 a 3) en condiciones relajadas. Posteriormente, los mismos ejercicios se realizaron nuevamente bajo un entorno estresante. El estrés se creó introduciendo factores físicos, auditivos e interrupciones.
Los resultados en habilidades técnicas fueron evaluados mediante la puntuación de relajación y estrés, así como el tiempo requerido para completar los ejercicios bajo condiciones de relajación y estrés. Se utilizó una métrica detallada para evaluar las variables en relación con las situaciones de estrés, incluyendo el estrés físico, la prisa, la presencia de música ambiental e interrupciones programadas.
Los resultados se expresan mediante la mediana y el rango intercuartílico. Para compararlos, se realizaron la prueba de Wilcoxon para muestras pareadas y la prueba U de Whitney. Los resultados se estratificaron por año de residencia (1-2 años vs. 3-4 años).
ResultadosLa puntuación de estrés fue significativamente menor en los tres ejercicios en comparación con la puntuación de relajación (75 vs. 86, 52 vs. 90, 55 vs. 61 respectivamente, p>0.05). El tiempo para realizar los ejercicios fue menos predecible y fue aún menor en situaciones estresantes sin diferencias estadísticas. Bajo estrés, tanto los residentes más jóvenes como los más avanzados obtuvieron peores puntuaciones en los ejercicios más complejos.
ConclusiónEl estrés afecta a la cirugía con simuladores. Los ejercicios más difíciles son los más propensos a ser afectados por el estrés. Estos resultados sugieren que a través de simuladores oftálmicos, los oftalmólogos tienen la oportunidad de entrenar el estrés quirúrgico y por lo tanto mejorar la seguridad del paciente.
It is well known that stress may play a crucial role in daily surgical activity. Interruptions, poor physical condition, time constraints, noise, and surgical complications can have a negative impact on surgical technical and psychomotor performance.1 By jeopardizing concentration capacity, it compromises decision-making process. Moreover, it can have consequences on tremor and handling of instruments.1–3
Negative emotions such as anxiety and worries, decrease working memory, attention, and decision-making.1 Several studies suggest a negative impact of surgeon fatigue on patient outcomes.1 The high noise level in the operating room seems to have a negative effect.4 Some study shows that experienced surgeons have less stress and less affected performance than less-experienced residents,5 and that fatigue seems to affect them less.6 Although these aspects are known, prospective randomized studies on the influence of stress have not been carried out because of obvious ethical reasons.
Recently, surgical simulators have been increasingly available in ophthalmology, mainly based on cataract and vitrectomy surgery. They have proven to be a useful tool for training, not only for ophthalmology residents, but also for acquiring or improving certain skills even for already experienced surgeons.7,8 It allows the progress in a comprehensive, faster, and more efficient way of the necessary skills for the development of basic and advanced procedures in ophthalmology, thus creating a better learning environment and improving costs.9 Simulators are becoming a new tool to achieve better results in surgical procedures and improving the quality of care.
The objective of this study is to evaluate the influence of stress factors on surgical procedures using an ophthalmology simulator and detect which exercises are more influenced.
Material and methodsStudy designA prospective study of a cohort of 13 residents was conducted at Vall Hebron University Hospital in Barcelona, Spain.
Study population and previous trainingThe study population consisted of residents undergoing training in ophthalmology at a hospital in Spain. All study participants underwent basic ophthalmic simulation-based surgical program training prior to the study to become acquainted with the simulator and the surgical exercises. This basic training consisted of performing and passing the 3 proposed exercises (E1, E2, and E3) along with other exercises according to their level.
E1 for first-, second-, and fourth-year residents was hydromaneuvers and for third year was anti-tremor. E2 for first- and second-year residents was anti-tremor, forceps training for third year, and for fourth year was bimanual manipulation. E3 for first-, second-, and fourth-year residents was capsulorhexis and for third year was bimanual manipulation.
To guarantee the knowledge of the simulator, at the baseline, all had to have passed the exercises with 60% success, at least twice. All participants knew the objectives of the study and provided informed consent. Nevertheless they did not know the types of stressors they were undergoing until minutes before performing the test under pressure.
Simulators and exercisesEyesi Surgical (Haag Streit®, Kioz, Suiss) were the used simulators in this study. Exercise programs were different according to residency level (E1, E2, and E3).
For first- and second-year residency, the following exercises were chosen to carry out the study: hydromaneuvers, anti-tremor, and capsulorhexis, with an increasing level of difficulty (capsulorhexis was more complex than hydromaneuvers). Second-year residents had a higher level of difficulty than first-year residents. These procedures were included in the cataract surgery simulator.
Third-year residents focused on vitreoretinal surgery within the vitrectomy simulator. The proposed exercises were anti-tremor, forceps training, and bimanual manipulation. Also with an increasing level of difficulty, where the most complex exercise was the bimanual manipulation.
Fourth-year residents focused on complicated cataract surgery and the proposed items were hydromaneuvers, bimanual manipulation, and capsulorhexis. Here also, the capsulorhexis was more complex than hydromaneuvers.
At the end of the exercise, a global score (out of 100) and duration time were reported automatically from the simulator as metrics of technical skills. Additionally, target achievement, efficiency, instrument handling, microscope handling, and tissue were also assessed. These latest were analyzed following a likert scale: no scoring, failing, poor, correct, average, good, and excellent.
Surgical conditionsOnce the basic training was completed, participants were invited to perform the proposed exercises under relaxed conditions.
Then, the same exercises were performed again under a stressful environment. The stressful environment was defined as the union of physical stress, haste, auditory stress, and interruptions.
Each component of the stressful environment was defined as follows. The physical stress was intended to produce an expected increase in adrenergic response with increase in heart rate and blood pressure. It was done by rapidly climbing the stairs to the simulation area (5 floors), just before starting the exercises. The time taken was approximately 1 min.
During the exercises, an observer kept a stopwatch in his hand commenting that time was running out and encouraging them to hurry up.
Auditory stress was caused by loud music played at a moderate volume level and the chosen songs were: “Killing in the name of” by Rage Against the Machine, “Tourette” from Nirvana and “Anarchy in the UK” from the Sex Pistols.
Moreover, in each of the exercises, the surgeon was interrupted to solve a simple math problem, 2-digit addition or subtraction, 1-digit multiplication and division.
The stress environment was conducted by the same person.
Statistical considerationsSince there are no previous similar studies, it was not possible to calculate the sample necessary to check our hypothesis. All available residents who agreed to participate were taken. The Wilcoxon test for paired samples was used for the comparison of scores and times. To compare both groups, the Whitney U test was used for independent samples. The results were stratified according to junior (first and second year) and seniors (third and four year).
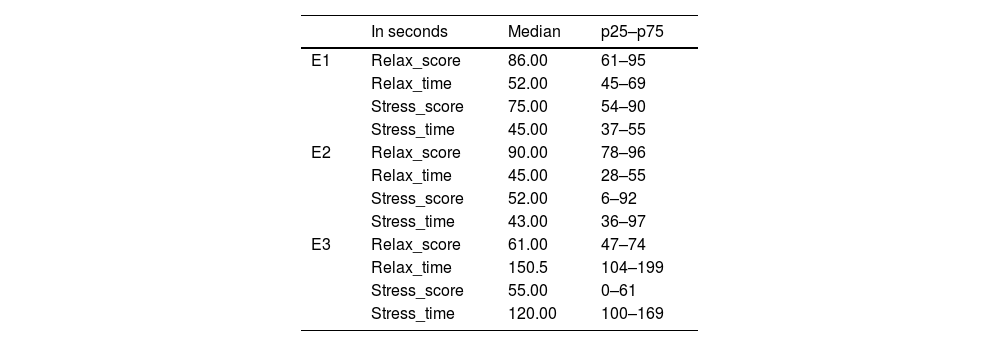
Results13 residents participated in the study. There were 3 first-year residents, 4 second-year residents, 4 third-year residents, and 2 fourth-year residents. E1, E2, and E3 refer to exercises 1, 2, and 3, respectivel,y under a relaxed and stress environment. Table 1 summarizes median and interquartile range of time and score in the 3 exercises under relaxed and stressed environment. As expected, the score under stressed environment was significantly lower in the 3 exercises (p>.05). Time to perform the test was less predictable and was even lower in stressful situations with no statistical differences.
Median and interquartile range in the 3 exercises: E1, E2, and E3 under relaxed and stressed environment.
| In seconds | Median | p25–p75 | |
|---|---|---|---|
| E1 | Relax_score | 86.00 | 61–95 |
| Relax_time | 52.00 | 45–69 | |
| Stress_score | 75.00 | 54–90 | |
| Stress_time | 45.00 | 37–55 | |
| E2 | Relax_score | 90.00 | 78–96 |
| Relax_time | 45.00 | 28–55 | |
| Stress_score | 52.00 | 6–92 | |
| Stress_time | 43.00 | 36–97 | |
| E3 | Relax_score | 61.00 | 47–74 |
| Relax_time | 150.5 | 104–199 | |
| Stress_score | 55.00 | 0–61 | |
| Stress_time | 120.00 | 100–169 |
E1: Exercise 1.
E2: Exercise 2.
E3: Exercise 3.
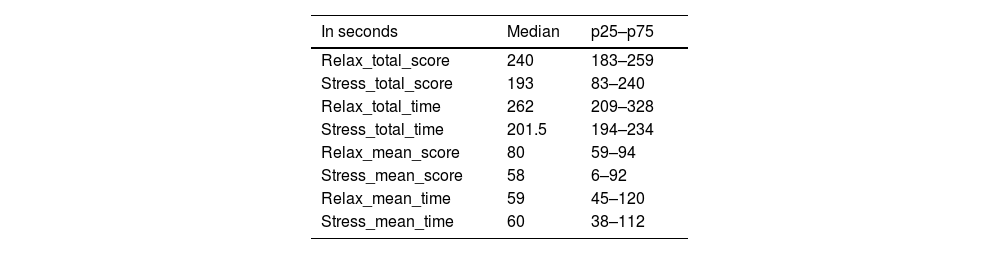
The total score (out of a maximum of 300) under relaxed environment was statistically higher than the score obtained in stress environment, 237 s versus 182 s (p>.05). Although there was a tendency for surgical times under stress to be shorter than times under relaxed environment, this difference was not statistically significant (247.5 s versus 208 s; p>.05 (Table 2).
Median and interquartile range of total score and time under relaxed and stressed environment.
| In seconds | Median | p25–p75 |
|---|---|---|
| Relax_total_score | 240 | 183–259 |
| Stress_total_score | 193 | 83–240 |
| Relax_total_time | 262 | 209–328 |
| Stress_total_time | 201.5 | 194–234 |
| Relax_mean_score | 80 | 59–94 |
| Stress_mean_score | 58 | 6–92 |
| Relax_mean_time | 59 | 45–120 |
| Stress_mean_time | 60 | 38–112 |
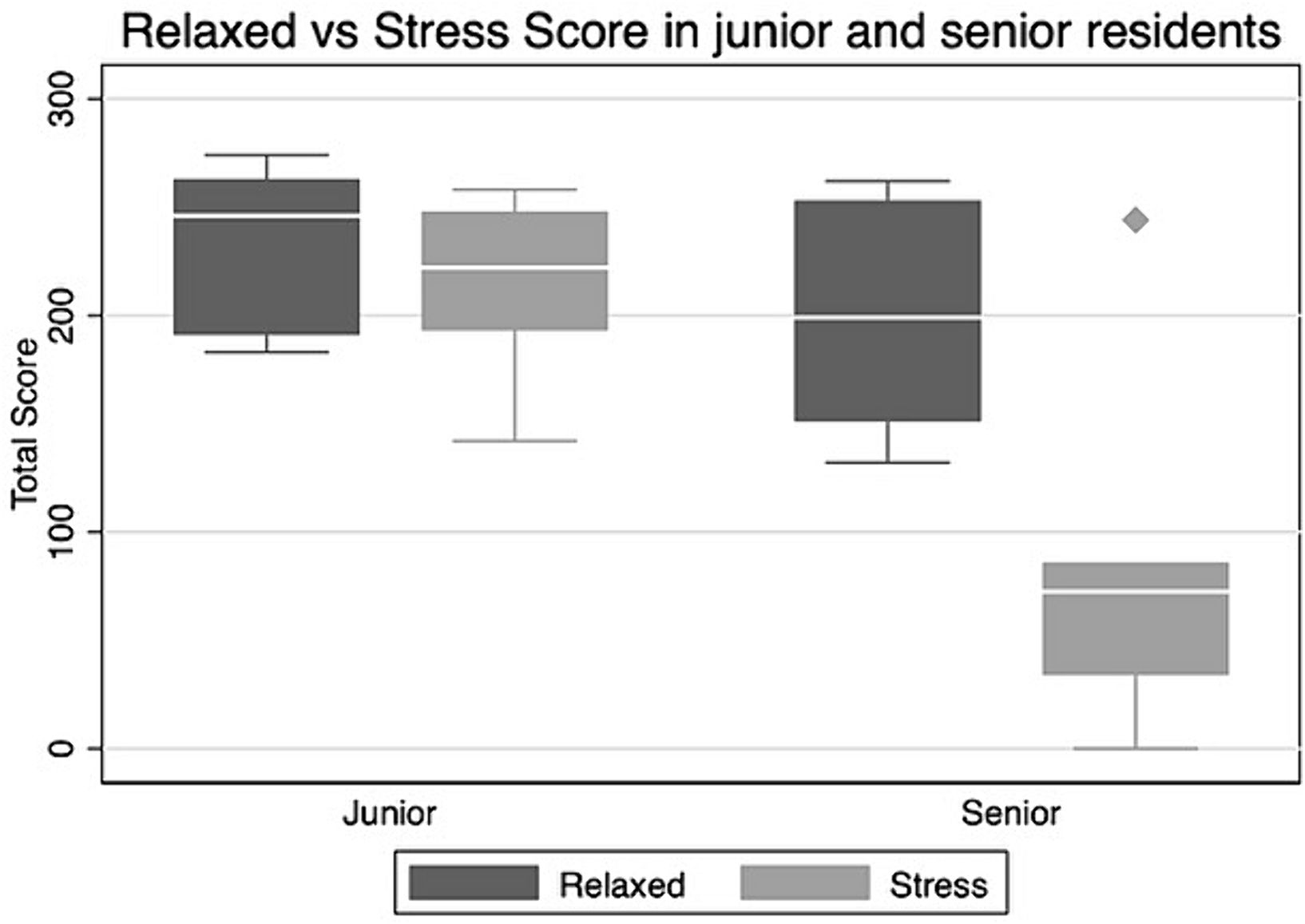
The participants were divided into juniors and seniors. There was a total of 7 juniors and 6 seniors. Total score under relaxed environment in junior and senior residents was 231 and 199, respectively, with no statistical differences. In the stressful environment, these differences were accentuated (217 in juniors and 84 in seniors), although it was not statistically significant either (Fig. 1).
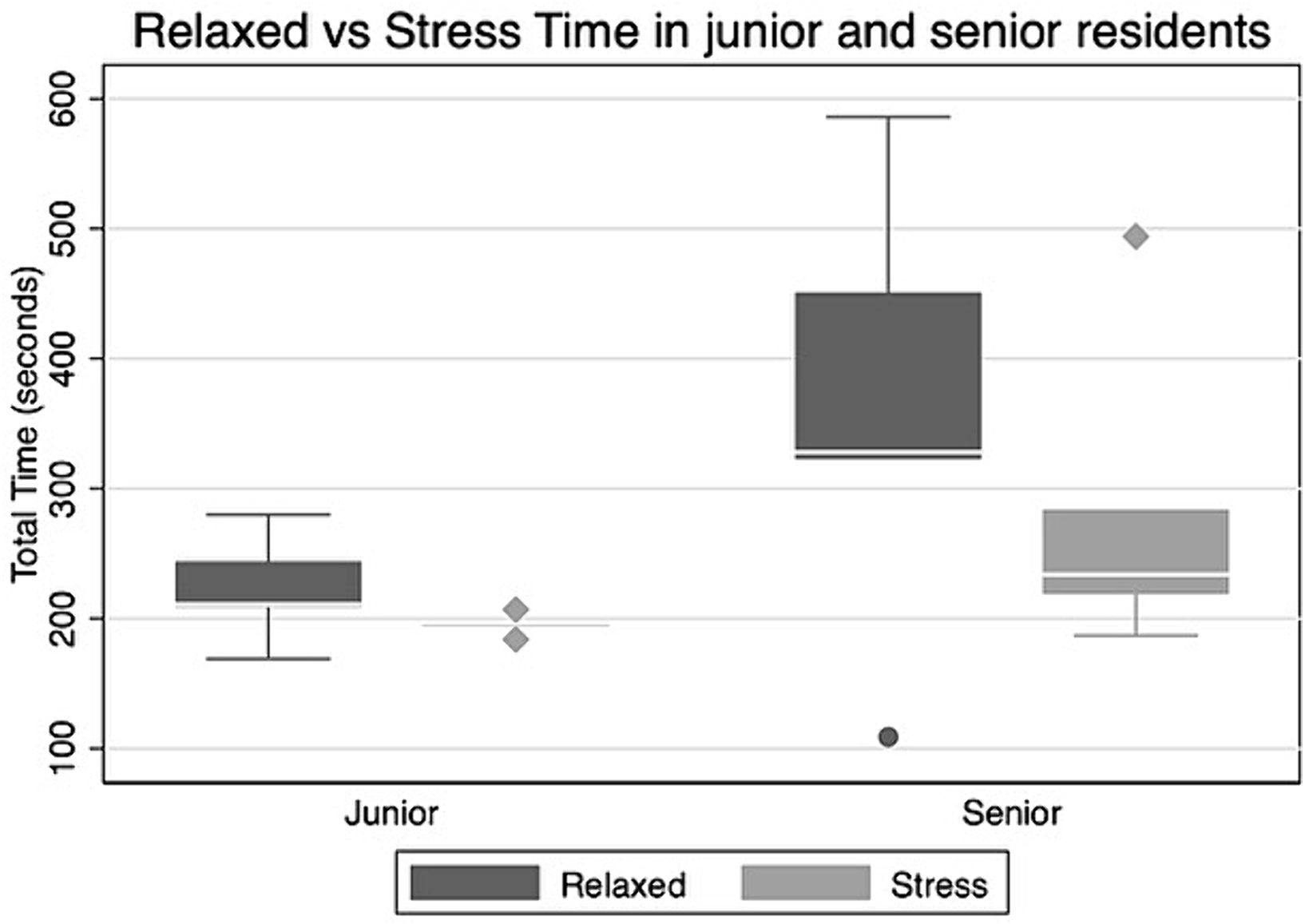
The mean time to perform the exercises was lower in the younger residents, 222 s under normal conditions and 195.4 s under stress conditions, compared to the 359 s it took for the older residents to complete the exercises at baseline and the 283.6 s it took to finish under stressful environment, although such differences were no significant in both cases (Fig. 2).
The score difference before and after the stress were very different between the groups. On average, the group of juniors decreased 13.3 points when performing the exercises under stress conditions, while the group of senior residents decreased 114.5 points (p=.0082).
The exercise that penalized young people the least was “hydromaneuvers” in which the average improved their qualifications under stress conditions (differential −0.42). The “capsulorhexis” exercise was the one that obtained the lowest scores in stress environment (12-point differential). The senior residents all obtained worse scores under stress, the exercises “forceps training” and “bimanual” were the ones that had the worst result and a greater variability between the subjects (differential 62.83 points).
DiscussionSurgical simulators may help in reducing the learning curve along the residency period, allowing the acquisition of surgical technical skills,7–9 particularly in stressful situations. Thus, facing unfavorable situations in simulation could be advantageous in managing these types of situations in daily clinical activity.10
Our study revealed a notable decrease in technical performance under stressful conditions, as evidenced by reduced scores in exercises requiring precision and dexterity. The impact of stress on technical skills is multifaceted, affecting various aspects of surgical performance such as instrument handling, maneuver accuracy, and overall efficiency. These findings underscore the importance of addressing stress management strategies tailored to enhancing technical competence among surgeons. The chosen stress conditions aimed to simulate, although exaggeratedly, what happens in many ophthalmology operating rooms. The first 2 refer to the rush and physical stress. Surgeons often carry out their daily activity under suboptimal conditions. Healthcare overload, the need to finish on time, and the presence of setbacks may contribute to cause significant discomfort in the surgeon and the rest of the team.6 Surgeons may come to operate in a hurry after daily rounds, traffic jams, or from attending incoming patients. These stressful situations have been attempted to be recreated, on one hand, with a minute of physical activity and, on the other hand, with the presence of an examiner timing and encouraging them to work faster. In analyzing the obtained results, it is imperative to consider that the stress induced by stair-climbing does not uniformly affect all participants, contingent upon their physical condition; nevertheless, it may impact all individuals similarly when timing the exercises. At no time was the chronometer time considered, since only the surgical time of the exercises provided by the equipment was counted. Residents could have calmly stopped between surgeries to relax without it affecting their scores, but none even considered that possibility. Contrary to what might be expected by starting to operate just after a minute of intense exercise, the first of the “hydromaneuvers” and “anti-tremor” exercises performed best under stressful conditions. A previous study by Taffinder et al. analyzing the effect of time pressure on the performance of a virtual laparoscopic task, revealed that time pressure had a detrimental effect on surgical precision.11
The third condition introduced in the study was auditory stress.4,12–14 Not always in operating rooms do we find the ideal sound conditions. Ventilation, electronics, and even lights can emit sounds, sometimes insidious and unpleasant. It is common for teams to play music, music radios, or playlists, with ups and downs in volume and with music that is not always relaxing. Finally, the level of loudness is greatly influenced by the personnel in the operating room and their conversations, assistant surgeons, residents, instrumentalists, anesthesiologists, anesthesia nurses, students, caretakers, and assistants. We do not always realize the number of people who can go through an operating room while operating. This condition has been simulated by loud music. The chosen songs seem to fulfill the objective both for their lyrics and for the important presence of drums, guitars, and screams; in fact, the use by the Central Intelligence Agency as torture of the chosen main song (“Killing in the name of”) is known. Arabacı et al.13 in their investigations of noise levels in operating rooms found that the anxiety levels and workload levels correlated positively with noise levels. Boghdady et al.12 in their systematic review concluded that a classic music when played with a low to medium volume could improve the surgical task performance and that the distracting effect of music should also be put in consideration when playing a loud or high-beat type of music.
The last condition chosen to simulate unfavorable conditions in the operating room are interruptions,15,16 again, something very frequent during surgeries, in our case, they have been simple arithmetic operations, which did not seem to entail great difficulty of resolution, but it is intended to simulate many of the interruptions surgeons experience: reminder about the patient waiting outside, call from the nursing supervisor to ask about instruments, and the anesthetist asking about the next surgery among others.
This study has shown that the score obtained in the simulator under stressed environment is significantly lower than under relaxed environment. Similarly, a previous study by Moorthy et al.17 analyzing the effect of adverse environmental conditions on laparoscopy surgical performance, found that a significantly higher number of errors occurred under stress-inducing conditions and that the effect was more pronounced when all the stressors were applied in combination.
The total score in juniors residents was higher than in seniors and with stress the difference was accentuated. In contrast, previous studies findings show that experienced surgeons had better technical performance on stress than novice surgeons.5,18 This could be explained by the fact that in our study, the senior residents performed more complex exercises than juniors, and from what we have seen in our results, the most complex exercises are the ones more affected by the stress.
The study has some limitations that must be considered when interpreting the results obtained. We consider that the small size of the sample (13 residents, all of them from the same center), is one of the main limitations it presents, given that a larger sample size and greater heterogeneity would add more value to the statistical significance of the results. Although in real conditions we face similar surgeries, each intervention and each step involves a difficulty and possible complications that are not reflected in the simulation. Some real stressors cannot be extrapolated to simulation studies, such as the patient's collaboration, sometimes related to the level of sedation or the pain threshold that they present; the surgical material itself, which sometimes varies or is not in ideal conditions; or errors caused by the rest of the operating room staff during the intervention, which also trigger stress and delays in surgery. Further validation of our assessment methods is needed to ensure the robustness and generalizability of our findings.
Stressful conditions seem to reduce surgical time both in novice surgeons and in more experienced surgeons, which is reflected in a clear decrease in the performance and final score of the exercises in both groups. In real life, a stressful surgical environment may promote hasty termination of procedures and can lead to complications that have irreversible visual consequences for the patient.
The greater the complexity of the exercises performed under stressful conditions, the more pronounced the decrease in their performance. This explains why many surgeons prefer to reduce the ambient sound or light in the operating room when dealing with more delicate procedures. Furthermore, the observed decrease in technical proficiency under stress highlights the need for targeted interventions aimed at mitigating stress-induced impairments in surgical technique. By incorporating stress management techniques into surgical training programs, such as mindfulness-based stress reduction or cognitive–behavioral interventions, surgeons may develop resilience and adaptability in high-pressure surgical environments.
Therefore, from what we have been able to demonstrate in this study, stress and external conditions can have a great influence on surgeons and on surgical exercises, as surgery requires the coordination of physical and cognitive skills, mainly affecting those of more complexity. Training through simulators for ophthalmologists allows improving surgical stress without harm to the patient.
Ethical considerationsAll participants voluntarily provided the informed consent. The data were collected anonymously, considering only the year of residency. The study was approved by the ethic committee of the hospital PR (AG) 112 / 2022.
The sources of the material used in the study was made with the hospital's own resources. Johnson & Johnson temporarily ceded the simulators.