To report the experience of minimally invasive spine surgery (MISS) training course in different languages and specialties for Latin American spine surgeons, and on their level of satisfaction with the curriculum.
MethodsA total of 29 hands-on training workshops were conducted over a period of 6 years, on using a MISS technique for degenerative disk disease. The participants completed two questionnaires aimed at evaluating the activities including the methodology, objectives, suitability of facilities, and instruments provided, as well as general satisfaction. Statistical analysis was performed using R 3.1.1 for Windows. Demographic and descriptive statistics were employed.
ResultsA total of 366 specialists took part and included neurosurgeons, orthopaedists, and anaesthesiologists. The questionnaire was answered by 249 medical doctors from 12 Latin American countries, 98% of which professed to be satisfied with the training activity.
ConclusionsThe use of educational tools, such as surgical simulators contributes to the new learning process techniques and adds confidence to the surgeons. The implementation of workshops conducted using strict planning leads to a high level of satisfaction among the participants, thus minimizing the differences between specialties or languages.
Presentar la experiencia lograda en el entrenamiento en técnicas mínimamente invasivas de columna para cirujanos de toda Latinoamérica con diferentes especialidades e idiomas, y reportar el grado de satisfacción con el currículo implementado.
MétodosSe realizaron un total de 29 entrenamientos durante 6 años en una técnica mínimamente invasiva de columna para el tratamiento de discopatía degenerativa. Los participantes respondieron 2 encuestas con el fin de evaluar el contenido curricular general de la actividad de entrenamiento. Se analizaron las encuestas empleando el programa R 3.1.1 para Windows.
ResultadosUn total de 366 especialistas realizaron el entrenamiento. Las especialidades entre los participantes fueron: neurocirujanos, ortopedas y anestesiólogos. Las encuestas fueron contestadas por un total de 249 médicos de 12 países de América Latina. El 98% de los encuestados avaló el modelo educativo y el currículo en general.
ConclusionesEl uso de herramientas educativas, como la simulación quirúrgica, contribuye a los procesos de entrenamiento de nuevas técnicas quirúrgicas y permite a los cirujanos lograr confianza para el momento en que tengan que realizarlas. La implementación de talleres de entrenamiento conducidos bajo un plan curricular permite un alto grado de satisfacción en los participantes, y minimiza las diferencias entre especialidades e idiomas.
The minimally invasive spine surgery (MISS) has offered new alternatives for the treatment of lumbar pain caused by discopathy, facet joint pain, stenosis and instability, showing effectiveness and safety when compared to the conventional surgery.1–4 This type of techniques has been gaining relevance in the spine surgeons practice around the world. The growth in number of surgical centers joining these techniques is evidenced in the increase of publications in specialized journals, from 14 articles published in 2000 to 5533 in 2016.5
MISS benefits and optimal results are highly related to factors such as an adequate choice of patient and a trained surgeon.6 Therefore, the technical ability and certainly the training of the surgeon play a key role in the clinical results. Skill development for implementing these surgical techniques demands time, patience, and perseverance from the surgeon.7 Notwithstanding its high importance, some aspects of the medical training are still carried out via obsolete processes; therefore, the percentage of training in patients remains high.
The urgent need to implement effective and efficient training processes has been identified; which do not import risks to patients, can be conducted away from the operation rooms (with their high associated costs), and are replicable and applicable to surgeons in different stages of their learning curve. Evidence of this need emerged from a study published in the late 20th century by the US Institute of Medicine, where close to 98,000 annual deaths were associated with medical errors.8 This statistic was summarized in an estimation indicating that the probability of dying at a hospital is ten times the probability of dying in a plane,9 this issue adds to the financial factor that estimated for 1997 a cost of USD 53 million related to the training of residents in surgical specializations in the US.10 These figures prove that Halsted's training method of “see one, do one, teach one” needs a previous complement by a series of teaching tools.
Animal and human cadaver specimens are highly effective tools in training processes,11,12 considered the gold standard for surgical skill development.13,14 The use of these instruments can become key to reducing the times in a learning curve and to improving the surgical competences in surgeons,15 and they should be used systematically before performing the procedures in patients. Taking into account their limited availability, cadavers can be complemented with easily accessible tools such as mechanical dry simulators, and thus the training activity effectiveness is maximized.
The purpose of this article is to show the six-year experience in a multispecialty learning processes that employ biological and mechanical simulators for the development of resident and non-resident spine surgeons’ surgical skills in a percutaneous technique of minimally invasive discectomy for the treatment of degenerative discopathies, and to show the participants’ degree of satisfaction with the method used.
MethodsParticipantsDuring March 2008 and March 2014, 29 hands-on workshops were held for training in a percutaneous technique of mechanical and thermal discectomy for discogenic lumbar pain treatment using the Disk Fx® system (Elliquence LLC, NYC). The activities were carried out in a surgical training center with exclusive facilities for medical education processes (CLEMI: Bogota, Colombia), employing as teaching tools class lectures, dry workshops (mechanical simulators) and workshops in human cadavers (biological simulators).
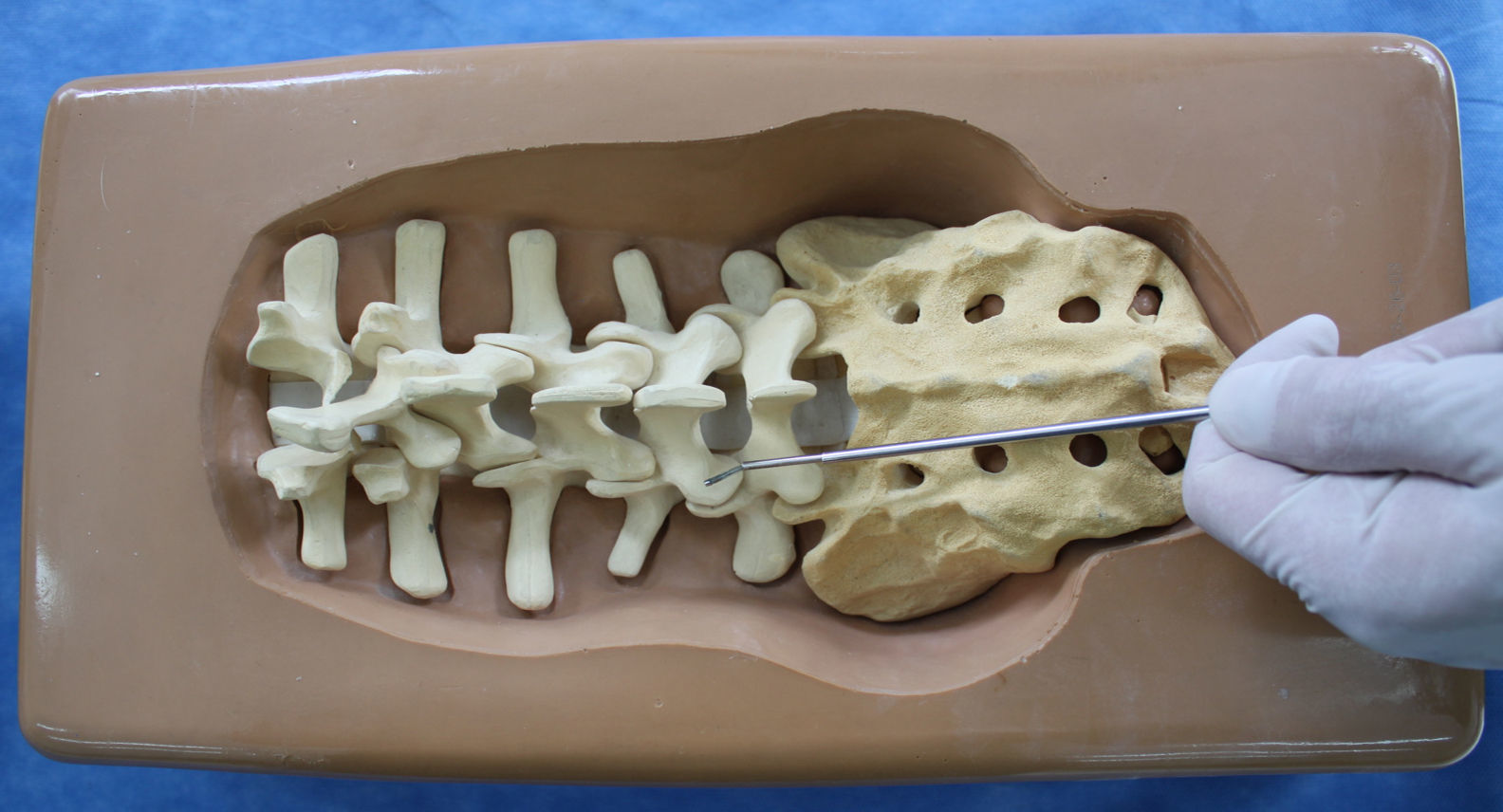
Workshop duration was one day (8h). All the activities were carried out in a similar sequence that comprised a brief theoretical contents — a review of the surgical anatomy and the technique description —; a dry workshop with commercially available mechanical simulators (Sawbones, Pacific Research Laboratories Inc., Vashon Island, WA) (Fig. 1) and a wet lab with fresh whole human cadavers — supplied by the training center — under a full concept of operating room (Fig. 2).
For each of the 29 workshops, 3–4 surgery tables were established for 2–4 participants each. The composition of the teams was determined by criteria as their affinity in surgical centers, their language (Spanish, Portuguese), and years of experience in conventional surgery.
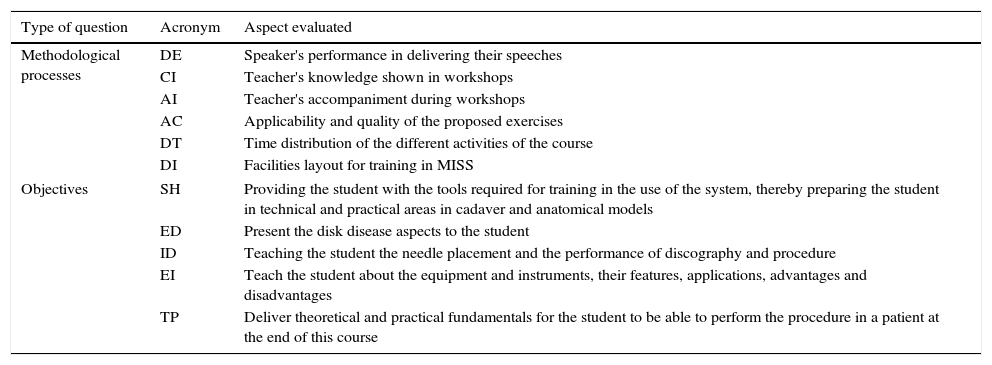
Study designWith the purpose of determining their experience and evaluating their satisfaction, at the beginning and at the end of the activity the participants were handed a questionnaire about their specialization, length of experience, type of previous training, fulfillment of their expectations with respect to the global course, methodological processes and workshop objectives (Table 1). The expectation fulfillment variable was a yes/no dichotomous question, whereas the questions about methodology and objectives were measured by an ordinal estimation scale where 1 corresponded to very unsatisfied and 5 to very satisfied.
Methodological aspects and fulfillment of objectives inquired from each of the workshop participants.
| Type of question | Acronym | Aspect evaluated |
|---|---|---|
| Methodological processes | DE | Speaker's performance in delivering their speeches |
| CI | Teacher's knowledge shown in workshops | |
| AI | Teacher's accompaniment during workshops | |
| AC | Applicability and quality of the proposed exercises | |
| DT | Time distribution of the different activities of the course | |
| DI | Facilities layout for training in MISS | |
| Objectives | SH | Providing the student with the tools required for training in the use of the system, thereby preparing the student in technical and practical areas in cadaver and anatomical models |
| ED | Present the disk disease aspects to the student | |
| ID | Teaching the student the needle placement and the performance of discography and procedure | |
| EI | Teach the student about the equipment and instruments, their features, applications, advantages and disadvantages | |
| TP | Deliver theoretical and practical fundamentals for the student to be able to perform the procedure in a patient at the end of this course | |
The complete curricula and description of the technique employed have been thoroughly described and published previously by the authors.16
Statistical analysisDemographic and descriptive statisticians were engaged. Statistical analysis was performed with R 3.1.1 for Windows.
ResultsThe total number of participants in the workshops was 366 specialists. Out of them, 249 fully completed both questionnaires. Three types of specialists participated in the training: orthopedics 56% (n=139), neurosurgery 43% (n=107), and anesthetics 1% (n=3). Table 2 specifies the distribution per countries.
Average previous experience of participants was 8.41 months (SD=8.99). 69.54% had less than 1 year of experience, 24.14% had between 12 and 24 months, and only 6.32% had more than 2 years of experience.
With respect to previous training, 38% of the surgeons did not have any type of training, 32% of the surgeons admitted having carried out a part of their training on another surgical technics -like open surgery- in patients, while the remaining 30% had trained with tools such as dry simulators (6%), animals (3%), and cadavers (20%).
As to overall course satisfaction, 98% (244/249) of the participants stated their satisfaction. About facilities, 92.5% recorded being very satisfied with the layout. In turn, all the methodological processes of the activity were rated between satisfied and very satisfied (4 and 5) above 97.6%, whereas “distribution of time” obtained the lowest satisfaction rate (DE, 99.2%; CI, 98.8%; AI, 99.2%; AC, 98.8%; DT, 97.6%).
Last, all the objectives attained a high satisfaction rate, 5 (very satisfied) from more than 80% of the participants, SH, 84.5%; ED, 80.3%; ID, 87.0%; EI, 87.0%; TP, 86.6%; and a 4 (satisfied) rate with values between 11.3% and 17.6%.
DiscussionThe degree of satisfaction in educational programs can become a major factor in training processes and is related with high confidence and perception of patient safety.17 This study describes the cadaver based training experience of a number of Latin American specialists in spine surgery, in a minimally invasive surgical technique for the treatment of lumbar degenerative discopathy. The results showed that a medical education program based on a mainly practical curricula with a timely accompaniment of suitable instructors, having a complete set of material and using (biological and mechanical) simulators as the main teaching tool, it is possible to obtain in the students a high degree of satisfaction (98%) for the general aspects of the program. In addition, the experience obtained high fulfillment of objectives and high satisfaction with the proposed methodology, as expressed by the rating greater to 4/5 in more than 97% of the participants.
A recent study conducted among neurosurgery residents showed a satisfaction rate greater than 65% by implementing cadaver training processes included in their specialization curriculum. Students also showed a clear preference for the use of cadavers as against other teaching tools such as books, dry models, videos or virtual media. Lastly, students did highly agree that cadaver training provides them with greater confidence, better preparation and ability to prevent intraoperative errors.17
An important finding was that the study showed that one in every three surgeons admitted to having performed some previous training on another technic in patients, a relatively low figure compared with other specializations placing it up to 69.6%,18 but relevant nevertheless. The reason of that difference could rely on the quite specific nature of the procedure, therefore, 38% of the participants argued that they did not have any type of training. Last, in this series, the length of previous experience of the participants showed a distinct preference by novice surgeons — near 70% — for the implementation of this type of innovative procedures.
Another remarkable result was that the workshops’ participants were from three different specialties and twelve nationalities — and thus, different languages —. Neurosurgery and orthopedics participation showed similar percentages in a 1:1.2 ratio. Also, the country with most participants was Brazil and although the course was taught in Spanish, the Brazilians’ satisfaction degree was 93% (74/76). This shows that language and specialty differences can be minimized with the implementation of a quality curriculum without an effect of these matters on the satisfaction.
Among the material aspects of the educational program, we must highlight two, the facilities’ suitability and the complete and appropriate surgical material. Foremost, one of the most important conclusions of a study by the American College of Surgeons (ACS) was that to withdraw training from “expensive” operating rooms is a requirement,19 entailing the availability of facilities enabled for conducting workshops that allow to maximize the accuracy of simulated processes. By contrast, the American Academy of Orthopaedics Surgeons (AAOS) showed that the US lacks surgical training centers for that specialty.20 The study evidently fulfilled two aspects, for the participants in the study reported a greater than 90% acceptance of the facilities provided, a result clearly related to the overall satisfaction with the process. Furthermore, the “Teach the student about the equipment and instruments, their features, applications, advantages and disadvantages” objective obtained one of the highest ratings across the sample with 98.7% of satisfied and very satisfied. This rate obeyed to the unqualified commitment of the industry to the training programs.
Among the limitations of the study, we should underline the absence of an objective evaluation parameter in skill development. This factor could be determinant to determine whether for this technique the simulated processes also shorten the learning curve, a criterion that has been validated in other techniques.19,21
It turns important to establish studies in future cases, which allow to establish whether or not for this specific technique the learning curve is actually shortened by the employment of simulated tools in early training stages. Likewise, it is important to compare different training models (video, dry simulators, cadavers, live surgery, patients) with the aim to identify which obtains the best results as to improvement of patients intervened subsequently.
As a conclusion, we assert that the use of simulation educational tools contribute to the new techniques learning process and allows building on the surgeons’ self-confidence. Training activities must be carried out upon proper planning, developing a distinct methodology and pursing specific objectives with the purpose of achieving high degrees of satisfaction. The elements that ensure a good learning process include suitable teachers and an appropriate infrastructure. As a last matter, we must recall that regardless of how accurate the simulation is (whether mechanical or biological), the classic Halsted model will not be eliminated, but rather it must become a complementing process in the learning curve.
Conflicts of interestDr. Ramírez, Dr. Rugeles and Dr. Ramírez are consultant for Elliquence. Dr. Alonso report no conflicts.
Research presented as e-poster on Fifth World Congress of Minimally Invasive Spine Surgery & Techniques 2016.