55 - EFFECT OF USTEKINUMAB MAINTENANCE THERAPY ON STOOL FREQUENCY AND RECTAL BLEEDING THROUGH 2 YEARS IN THE UNIFI PHASE 3 STUDY IN ULCERATIVE COLITIS
1Nancy University Hospital, Université de Lorraine, Nancy (France). 2University of Miami Miller School of Medicine, Miami, FL (USA). 3Humanitas Research Hospital, Milan (Italy). 4Janssen Research & Development, LLC, Spring House, PA (USA). 5The University of New South Wales and Macquarie University (Australia). 6Auckland City Hospital, University of Auckland (New Zealand). 7University of Calgary, Calgary, AB (Canada). 8University of California San Diego, La Jolla, CA (USA).
Introduction: The UNIFI randomized-withdrawal maintenance study evaluated subcutaneous (SC) ustekinumab (UST) in patients (pts) with moderately to severely active ulcerative colitis (UC). Pts who completed the maintenance study (WK44) could enter a long-term extension (LTE) through 220 weeks (wks). We evaluated the effect of UST maintenance therapy on stool frequency & rectal bleeding through 92wks.
Methods: Pts were eligible to dose adjust (PBO to q8w; q12w to q8w; q8w to q8w [sham dose adjustment]) starting at Wk56 and the recorded number of stools and rectal bleeding symptoms for 7 days before each visit. Proportions of pts with Mayo stool frequency subscores of 0 (normal number of stools) or 1 (1-2 stools more than normal) or rectal bleeding subscores of 0 (no blood seen) were evaluated. Absolute stool number was summarized.
Results: Pts in LTE included UST 90 mg q12w: n = 141 and UST 90 mg q8w: n = 143. Absolute stool number in UST q12w and q8w groups were 6.6 & 6.5 stools/day, respectively, at induction baseline and decreased to 2.8 and 2.7, respectively, by maintenance baseline. Reductions achieved at maintenance baseline were maintained at Wk92 (2.7 & 2.2, respectively). At induction baseline, only 12.8% & 18.2% of pts, respectively, had Mayo stool frequency subscores of 0 or 1. By maintenance baseline, 80.9% & 80.4%, respectively, had Mayo stool frequency subscores of 0 or 1, and these were maintained through Wk92 (79.4% & 86.7% at Wk92, respectively). At induction baseline, 9.2% & 7.0%, respectively, had no blood seen in the stool (Mayo rectal bleeding subscore of 0). By maintenance baseline, 87.2% & 84.6%, respectively, had no blood seen in the stool & these were maintained through Wk92 (86.5% & 88.8%) (table).
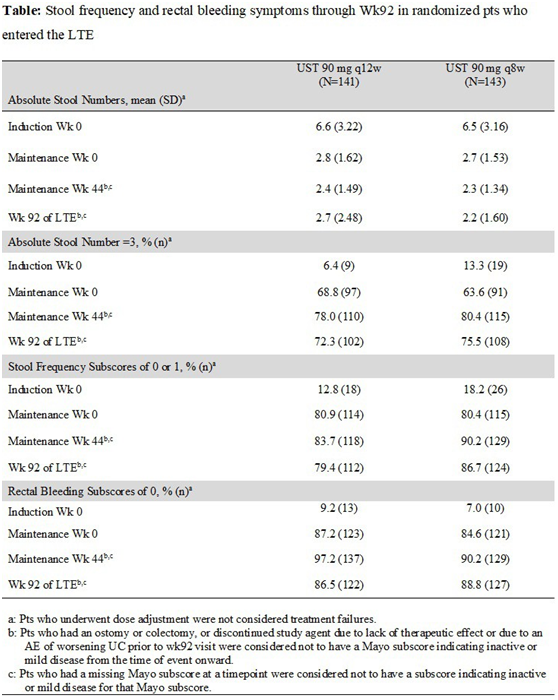
Conclusions: Among pts in the LTE, reductions in stool frequency and rectal bleeding achieved after IV UST induction were maintained through 2 years of UST SC maintenance. These data support the durability of response to UST in UC.